Self-reflection: Foundation for meaningful nursing practice
- Pattern recognition
- Similarity recognition
- Common sense and understanding
- Skilled know-how
- A sense of salience
- Deliberate rationality
- mental health
- RNL Feature

This site uses cookies to keep track of your information. Learn more here . Accept and close .
- Click here - to use the wp menu builder

- Privacy Policy
- Refund Policy
- Terms Of Service
- Nursing notes PDF
- Nursing Foundations
- Medical Surgical Nursing
- Maternal Nursing
- Pediatric Nursing
- Behavioural sciences
- BSC NURSING
- GNM NURSING
- MSC NURSING
- PC BSC NURSING
- HPSSB AND HPSSC
- Nursing Assignment

Reflective Practice in Nursing: A Guide to Improving Patient Care
Reflective Practice in Nursing: A Guide to Improving Patient Care -Reflective practice is an important aspect of nursing that involves the critical analysis of one’s own experiences and actions to improve nursing practice. It is a process of self-reflection and self-evaluation that can lead to personal and professional growth. This article will explore the concept of reflective practice in nursing, its importance in nursing practice, and the strategies and tools that can be used to facilitate reflective practice.
Table of Contents
Understanding Reflective Practice
The definition and concept.
Reflective practice refers to the intentional process of evaluating one’s experiences, thoughts, and actions to gain a deeper understanding of their impact. In nursing, it’s about analyzing the why and how behind every action taken, allowing for a comprehensive assessment of one’s performance.
Historical Context
The roots of reflective practice in nursing can be traced back to the work of influential theorists like Donald Schön, who emphasized the significance of “reflection-in-action” and “reflection-on-action.” These concepts laid the foundation for integrating self-reflection into nursing practice.
Concept of Reflective Practice in Nursing
Reflective practice in nursing is a process of self-reflection and self-evaluation that involves analyzing one’s own experiences and actions to improve nursing practice. It is a way of learning from experiences, both positive and negative, to improve future practice. Reflective practice is based on the assumption that nurses can improve their practice by reflecting on their experiences and critically analyzing their own actions.
Importance of Reflective Practice in Nursing
Reflective practice is important in nursing practice for several reasons. Firstly, it helps nurses to improve their practice by identifying areas for improvement and developing strategies to address them. Secondly, it can enhance nurses’ critical thinking skills by encouraging them to analyze their own experiences and consider different perspectives. Thirdly, it can promote self-awareness and personal growth by encouraging nurses to reflect on their own values and beliefs and how they influence their practice .
There are many benefits to reflective practice in nursing. It can help nurses to:
- Improve patient care outcomes
- Develop critical thinking skills
- Enhance communication skills
- Increase self-awareness
- Promote professional growth and development
- Cope with stress and burnout
Strategies and Tools for Facilitating Reflective Practice
There are several strategies and tools that can be used to facilitate reflective practice in nursing. Some of these include:
- Journaling: Journaling is a common tool used in reflective practice. Nurses can use a journal to record their thoughts and experiences, and then reflect on them to identify areas for improvement.
- Critical Incident Analysis: Critical incident analysis involves reflecting on a specific event or experience in practice and analyzing it to identify strengths and areas for improvement.
- Reflection on Action and Reflection in Action: Reflection on action involves reflecting on past experiences and analyzing them to identify areas for improvement. Reflection in action involves reflecting on experiences as they are happening and making adjustments to practice in real time.
- Peer Reflection: Peer reflection involves discussing experiences and actions with colleagues to gain different perspectives and insights.
- Feedback: Feedback from colleagues, supervisors, and patients can be a valuable tool for reflective practice, providing insight into areas for improvement.
- Professional Development: Professional development activities, such as attending conferences and workshops, can provide opportunities for nurses to learn and reflect on their practice.
Implementing Reflective Practice
Models of reflective practice.
Several models guide nurses through the reflective process. The Gibbs’ Reflective Cycle, for instance, involves stages like description, feelings, evaluation, analysis, conclusion, and action plan. These models provide a structured framework for introspection.
Steps in the Reflective Process
- Description: Recount the situation or experience in detail.
- Feelings: Examine your emotions during the event.
- Evaluation: Assess the positives and negatives of the situation.
- Analysis: Dig deeper into the factors influencing your actions.
- Conclusion: Sum up the insights gained from reflection.
- Action Plan: Define steps for future improvements.
Example of Reflective Practice in Nursing
As a registered nurse working in a busy hospital, I recently had an experience that highlighted the importance of reflective practice in improving patient communication and overall care. This incident prompted me to consider my approach to patient interactions and how it could be refined for better outcomes.
In this particular situation, I was assigned to care for a patient who was admitted for a complex surgical procedure. The patient, Mrs. Johnson, appeared anxious and had numerous questions about the upcoming surgery. Due to the high patient load, I felt a sense of time pressure and inadvertently rushed through her questions, providing concise answers without fully addressing her concerns.
Later that day, I engaged in reflective practice, realizing that my approach might not have been the most effective way to support Mrs. Johnson during such a critical time. I used the Gibbs’ Reflective Cycle to guide my self-examination:
- Description: I recalled the interaction with Mrs. Johnson and the rushed manner in which I answered her questions.
- Feelings: I acknowledged that my actions might have contributed to her anxiety and dissatisfaction.
- Evaluation: I assessed the negative impact of my approach on patient communication and the potential consequences for her overall well-being.
- Analysis: I delved into the factors that influenced my behavior, such as time constraints and a high workload.
- Conclusion: I concluded that while these factors were present, they should not have compromised the quality of patient care and communication.
- Action Plan: I determined that in future interactions, I would allocate dedicated time to address patient concerns, ensuring they feel heard and valued.
This reflective process led me to take actionable steps to improve my patient communication skills. In subsequent interactions with Mrs. Johnson, I intentionally created a calm and attentive environment. I provided her with detailed explanations about the surgery, and potential outcomes, and addressed her concerns with empathy. I also encouraged her to ask questions and clarified any doubts she had.
The impact of this reflective practice was profound. Mrs. Johnson’s anxiety visibly decreased, and she expressed gratitude for the time I spent addressing her concerns. Her positive feedback not only boosted her confidence but also reminded me of the significant role effective communication plays in fostering trust between nurses and patients.
This experience taught me that reflective practice isn’t just a theoretical concept but a practical tool that can transform patient care. By taking the time to analyze our interactions, understand our emotions, and make conscious efforts to improve, nurses can create meaningful connections with patients and enhance their overall well-being.
Barriers to Reflective Practice
Despite the importance of reflective practice in nursing, there are several barriers that can make it difficult to implement. Some of these include:
- Time constraints: Nurses may feel that they do not have enough time to engage in reflective practice due to heavy workloads.
- Lack of support: Nurses may not receive support from colleagues or supervisors for engaging in reflective practice.
- Fear of judgment: Nurses may feel uncomfortable reflecting on their experiences and actions for fear of being judged.
- Lack of training: Nurses may not have received adequate training in reflective practice, making it difficult to engage in the process.
Reflective practice is an important aspect of nursing that can lead to personal and professional growth. It involves the critical analysis of one’s own experiences and actions to improve nursing practice. Strategies and tools for facilitating reflective practice include journaling, critical incident analysis, peer reflection, and professional development. However, there are several barriers that can make it difficult to implement reflective practice, including time constraints, lack of support, fear of judgment, and lack of training. Despite these barriers, it is important for nurses to engage in reflective practice to improve their practice and promote positive patient outcomes.
Please note that this article is for informational purposes only and should not substitute professional medical advice.
LEAVE A REPLY Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Recent articles
4 basic techniques of physical examination in nursing., duties and responsibilities of midwife, multifoetal pregnancy complications nursing interventions, typhoid fever care plan, nursing course admission eligibility, what is the cause of cleft palate, download nursing notes pdf, male and female reproductive system pdf, human skeletal system nursing, staff nurse syllabus and exam pattern question bank -ii, pgi staff nurse exam question bank -1, anatomy and physiology of female reproductive system, human physiology digestion and absorption, anatomy and physiology the cardiovascular system nursing notes, hpssc staff nurse exam study material, more like this, what is a nursing diagnosis, what is acute care: a comprehensive guide, the importance of genetics in nursing, the role and qualities of mental health and psychiatric nurses, mental health nursing diagnosis care plan pdf, child pediatric health nursing notes -bsc nursing, mid-wifery pdf notes for nursing students, national health programmes in india pdf, reproductive system nursing notes pdf, primary health care nursing notes pdf, psychology note nursing pdf, nursingenotes.com.
- STUDY NOTES
- SUBJECT NOTES
A Digital Platform For Nursing Study Materials
Latest Articles
How nurses help the community, gifts for nursing home residents, gift ideas for nursing students, most popular.
© Nursingenotes.com | All rights reserved |
- Open access
- Published: 16 March 2023
Effectiveness of a critical reflection competency program for clinical nurse educators: a pilot study
- Sujin Shin 1 ,
- Inyoung Lee 2 ,
- Jeonghyun Kim 3 ,
- Eunyoung Oh 4 &
- Eunmin Hong 1
BMC Nursing volume 22 , Article number: 69 ( 2023 ) Cite this article
18k Accesses
9 Citations
Metrics details
Critical reflection is an effective learning strategy that enhances clinical nurses’ reflective practice and professionalism. Therefore, training programs for nurse educators should be implemented so that critical reflection can be applied to nursing education. This study aimed to investigate the effects of a critical reflection competency program for clinical nurse educators on improving critical thinking disposition, nursing reflection competency, and teaching efficacy.
A pilot study was conducted using a pre- and post-test control-group design. Participants were clinical nurse educators recruited using a convenience sampling method. The program was conducted once a week for 90 min, with a total of four sessions. The effectiveness of the developed program was verified by analyzing pre- and post-test results of 26 participants in the intervention group and 27 participants in the control group, respectively. The chi-square test, independent t-test, Mann-Whitney U test, and analysis of covariance with age as a covariate were conducted.
The critical thinking disposition and teaching efficacy of the intervention group improved after the program, and the differences between the control and intervention groups were statistically significant (F = 14.751, p < 0.001; F = 11.047, p < 0.001). There was no significant difference in the change in nursing reflection competency between the two groups (F = 2.674, p = 0.108).
The critical reflection competency program was effective in improving the critical thinking disposition and teaching efficacy of nurse educators. Therefore, it is necessary to implement the developed program for nurse educators to effectively utilize critical reflection in nursing education.
Peer Review reports
The critical thinking of clinical nurses is essential for identifying the needs of patients and providing safe care through prompt and accurate judgment [ 1 , 2 , 3 ]. Critical thinking can be practiced through critical reflection [ 4 ], a dynamic process in which nurses reflect on their nursing behavior to improve their perspective on a situation and change future nursing practices in a desirable direction [ 5 ]. Through critical reflection, nurses grasp the contextual meaning of a situation and reconstruct their experiences to apply their learning in practice, thereby identifying the meaning of nursing [ 3 ]. In other words, critical reflection can help nurses convert their experiences into practical knowledge [ 6 ]. Thus, critical reflection may be an effective learning strategy linking theory and practice in clinical nursing education [ 7 ].
Studies have reported that critical reflection is effective in improving nurses’ reflective practices and professionalism. Teaching methods that use critical reflection can improve nurses’ knowledge, communication skills, and critical thinking abilities [ 1 , 8 , 9 ]. These methods can be effective in improving clinical judgment and problem-solving abilities by providing new nurses with opportunities to apply their theoretical knowledge in clinical practice [ 10 , 11 ]. In addition, critical reflection has positive effects on the professionalism of new graduate nurses and reduces reality shock during the transition from university to clinical practice [ 12 ]. These advantages have led to the increasing application of critical reflection in training programs for new graduate nurses, including nursing residency programs [ 13 , 14 , 15 ].
In order to facilitate new nurses’ reflective thinking and practice by clinical nurse educators, educators must be trained to strengthen their critical thinking disposition, nursing reflection, and teaching efficacy competency. Educators help new nurses adapt and develop their expertise in clinical settings [ 16 , 17 ]. Moreover, continuing education for nurses to improve their teaching competency relates to the satisfaction of learners and nurse educators, which improves the quality of clinical nursing education [ 18 ]. Therefore, opportunities for nurse educators to develop teaching competency for critical reflection in education should be provided [ 19 ] and educational support for nurse educators to improve critical reflection competency is needed.
However, although there have been studies that have evaluated the effectiveness of the educational interventions concerning critical reflection to new nurses, few studies have been conducted on educational interventions on the critical reflection competencies of clinical nurse educators in charge of educating new nurses. Therefore, this study aimed to investigate the effects of a critical reflection competency program for clinical nurse educators on improving critical thinking disposition, nursing reflection competency, and teaching efficacy.
Study design
A pilot study was conducted with a pre- and post-test control group design to investigate the effects of the critical reflection competency program on the critical thinking disposition, nursing reflection competency, and teaching efficacy of nurse educators. The conceptual framework in this study was proposed that the critical reflection competency program will improve critical thinking disposition, nursing reflection, and teaching efficacy of clinical nurse educators [Fig. 1 ].
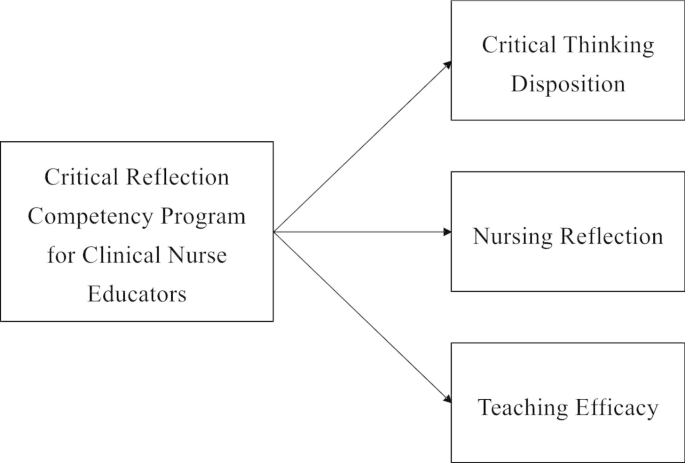
Conceptual Framework
Participants were clinical nurse educators in hospitals who were recruited using a convenience sampling method. Nurse educators were eligible to participate if they had dedicated nursing education in a clinical setting. They dedicated to nursing education focused on staff development of current nurses, especially the education for new nurses. They also included those who completed all four sessions of the program and participated in the data collection before and after the program. A recruitment document was sent to hospitals to recruit the participants, hospitals were selected with concerning role of clinical nurse educators. Participants were recruited from two hospitals of different sizes and the number of participants differed for each hospital, and they were allocated according to the order of registration.
The sample size required for the analysis was calculated using the G* Power 3.1.9.4. program with an effect size of 0.80, a significance level of 0.05, and a power of 0.80, following the literature [ 20 ]. By applying a self-reflection program for intensive care unit nurses [ 20 ], we calculated the effect size as large. Both the intervention and control groups required 26 participants. Considering a dropout rate of 20%, a total of 63 participants, including 32 in the intervention group and 31 in the control group, were recruited. From the intervention group, six participants who participated in the pre-test and completed all programs, but did not participate in the post-test, were excluded. In the control group, four participants who participated in the pre-test but not in the post-test were excluded. Thus, 26 and 27 participants in the intervention and control groups, respectively, were included in the final analysis [Fig. 2 ]. The pre-test for both groups was conducted in May 2021. Post-tests for the two groups were performed four weeks after the pre-test.
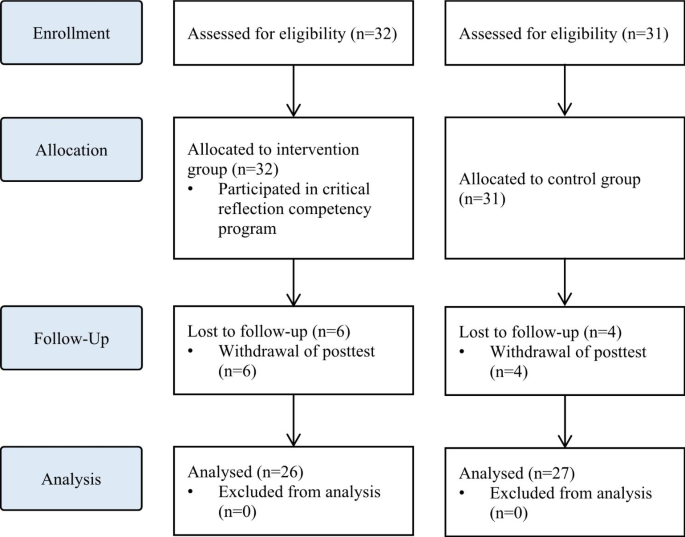
Flowchart of the study
Intervention
The intervention was developed and delivered by the first author, who has more than 15 years of teaching experience in nursing education, including critical reflection. The intervention was conducted between May 2021 and June 2021. Following previous studies that applied critical reflection in medical education [ 21 , 22 ], the intervention was conducted once a week for 90 min, with a total of four sessions. Owing to COVID-19, real-time online sessions were used to minimize contact between participants working in medical institutions. Every week before the sessions, the contents of the session, schedule, and Uniform Resource Locator (URL) were sent to participants via e-mail.
The intervention consisted of the following three steps in four sessions: (1) understanding critical reflection, (2) strategies to use critical reflection, and (3) practical uses of critical reflection [Fig. 3 ]. Synchronous online lectures were conducted in the first and second sessions. The contents of the first session included understanding of critical reflection and the clinical judgment process through critical reflection. Based on the content of the first session, the second outlined educational strategies using critical reflection in nursing education and the direction of critical reflection. In the third and fourth sessions, clinical nurses with experience of critically reflecting on themselves were invited as guest speakers to share their experiences and facilitate online discussions. Online discussions were also conducted in real time, and feedback from guest speakers and the author was immediately provided.
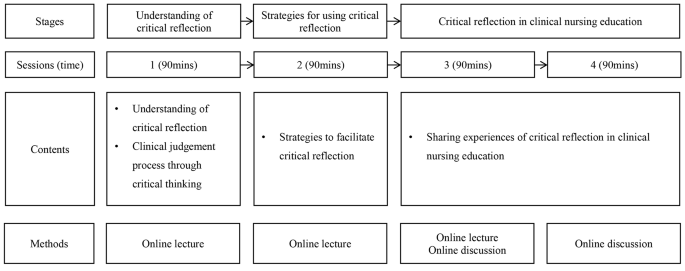
Critical reflection program for clinical nurse educators
Online self-report surveys were conducted before and after the program to assess the program’s effects. In both pre- and post-tests, critical thinking disposition, nursing reflection competency, and teaching efficacy were assessed, as well as information about participants, such as gender, age, experience in nursing education, and the type of institution and the number of beds they affiliated with.
Critical thinking disposition was measured using Yoon’s Critical Thinking Disposition Scale [ 23 ]. This scale comprises 27 items: 5 on “intellectual eagerness/curiosity,” 4 on “prudence,” 4 on “self-confidence,” 3 on “systematicity,” 4 on “intellectual fairness,” 4 on “healthy skepticism,” and 3 on “objectivity.” The items were evaluated on a five-point Likert scale (one point for “strongly disagree” to five points for “strongly agree”); a higher score indicated greater critical thinking disposition. The scale has good reliability as evidenced by a Cronbach’s alpha of 0.84 at the time of the development versus the reliability of the scale in this study was Cronbach’s alpha of 0.78.
Nursing reflection competency was assessed using the Nursing-Reflection Questionnaire, developed by Lee et al. [ 24 ]. This scale comprises four factors with 15 items, including 6 items on “review and analysis nursing behavior,” 5 on “development-oriented deliberative engagement,” 2 on “objective self-awareness,” and 2 on “contemplation of behavioral change.” Each item was evaluated on a five-point Likert scale (one point for “strongly disagree” to five points for “strongly agree”), with a higher score indicating greater nursing reflection competency. The scale has good reliability as evidenced by a Cronbach’s alpha of 0.86 at the time of the development versus the reliability of the scale in this study was Cronbach’s alpha of 0.82.
Teaching efficacy was evaluated using the Teaching Efficacy Scale developed by Park and Suh [ 25 ] to evaluate clinical nursing instructors. This scale consisted of six sub-factors with 42 items, including 12 items on “student instruction,” 9 on “teaching improvement,” 7 on “application of teaching and learning,” 7 on “interpersonal relationship and communication,” 4 on “clinical judgment,” and 3 on “clinical skill instruction.” Each item was evaluated on a five-point Likert scale (one point for “strongly disagree” to five points for “strongly agree”), with a higher score indicating greater teaching efficacy. The scale has good reliability as evidenced by a Cronbach’s alpha of 0.97 at the time of the development versus the reliability of the scale in this study was Cronbach’s alpha of 0.93.
Ethical considerations
This study was approved by the Institutional Review Board (IRB) of Ewha Womans University (IRB no. ewha-202105-0022-02). The need of written informed consent was exempted by IRB of Ewha Womans University. All methods were performed in accordance with the relevant guidelines and regulations. A description of the study, including its purpose, methods, and procedures, was posted on an online pre-test survey. Only those participants who agreed to participate were allowed to complete the questionnaire. The participants were also informed that they could withdraw from the study at any time and that the data of withdrawn participants would not be included in the final analysis. After the survey was completed, a mobile gift voucher was provided to those who agreed to provide their mobile phone number. Data were collected by researchers who did not participate in the program.
Data analysis
The collected data were analyzed using SPSS for Windows (version 28.0). Non-normally distributed data were analyzed using non-parametric tests. Descriptive statistics were used to calculate the frequency, percentage, mean, and standard deviation of participants’ general and institutional characteristics. Chi-square, independent t-, and Mann-Whitney U tests were conducted to test the homogeneity of the general characteristics and pre-test scores. The Shapiro-Wilk test was conducted to test the normality of the data. To test the difference between the pre- and post-tests for each group, analysis of covariance (ANCOVA) was used. As there was a significant difference in age between the intervention and control groups, an ANCOVA with age as a covariate was conducted for the difference in changes in test scores between the pre- and post-test.
Homogeneity test of general characteristics and dependent variables
All participants were female, with a mean nursing education experience of 27 and 23 months in the intervention and control groups, respectively. The homogeneity test of general and institutional characteristics, such as gender, nursing education experience, affiliated institution types, and the number of beds, were not statistically significant. However, the age differed significantly between the two groups. In the test for homogeneity of the pre-intervention scores, there were no significant differences in critical thinking disposition, nursing reflection competency, or teaching efficacy between the two groups, suggesting homogeneity of the dependent variables between the groups [Table 1 ].
Effects of critical reflection competency program
The effects of the critical reflection competency program are shown in Table 2 .
In the post-intervention phase, scores of critical thinking disposition, nursing reflection competency, and teaching efficacy all improved compared to the pre-intervention phase, and were higher in the experimental group than in the control group. The critical thinking disposition scores before and after the intervention were 3.61 ± 0.26 vs. 3.87 ± 0.04 in the intervention group and 3.76 ± 0.21 vs. 3.77 ± 0.04 in the control group, respectively. The nursing reflection competency scores before and after the intervention were 57.00 ± 3.42 vs. 60.86 ± 0.95 in the intervention group and 59.63 ± 5.24 vs. 59.04 ± 0.89 in the control group. The teaching efficacy scores before and after the intervention were 157.04 ± 10.60 vs. 171.98 ± 2.54 in the intervention group and 161.59 ± 14.77 vs. 160.48 ± 2.46 in the control group.
Age, which was significantly different between the intervention and control groups, was treated as a covariate to conduct the ANCOVA. The changes in critical thinking disposition (F = 14.751, p < 0.001) and teaching efficacy (F = 11.047, p < 0.001) scores were significantly different between the two groups. However, there was no significant difference in the change in the nursing reflection competency (F = 2.674, p = 0.108) score between the two groups.
Reflective practice is crucial to clinical nurses’ professionalism. Reflective practice enables positive learning experiences through deep and meaningful learning, and is essential for integrating theory and practice. It also enables nurses to implement what they have learned into practice, understand their expertise, and develop clinical competencies [ 26 ]. In this respect, it is important for clinical nursing educators to have critical reflection competencies and promote experiential learning among new nurses. In this study, a critical reflection competency program was developed to enhance clinical nurse educators’ critical thinking and teaching competency.
This program was effective in improving critical thinking disposition. In interventions for critical reflection, various aspects, including the introduction of critical reflection and guidelines to promote critical reflection, such as small group discussions and feedback, can be considered [ 27 ]. The program reflected these aspects and helped improve participants’ critical thinking disposition. In the third and fourth sessions, synchronous discussions on sharing experiences of critical reflection were effective. This is consistent with previous studies in which discussions improved reflective competencies [ 21 , 28 ]. Therefore, sharing experiences in the discussion section should be a key element of future educational interventions for critical reflection competency.
Furthermore, the program was effective in improving teaching efficacy. Teaching efficacy is the instructor’s belief in one’s own ability to organize and implement teaching [ 29 ], and is closely related to age, clinical experience, educational experience, professional development, and teaching competency [ 30 , 31 , 32 ]. Nurses who are more clearly aware of their roles as instructors tend to exhibit higher confidence in their teaching abilities [ 33 , 34 ]. That is, the participants in this study were clearly aware of their roles and developed confidence by sharing their educational experiences about critical reflection.
However, the program did not have a significant effect on nursing reflection competencies. In a previous study [ 10 ], reflective practitioners (RPs) received four weeks of critical reflection training and trained new nurses for six months. During training, new nurses wrote critical reflective journals and RPs provided feedback and shared their experiences. In this study, it seems that the methods and frequency of using critical reflection in nursing education varied for each participant, resulting in insignificant results for nursing reflection competency. It is necessary to provide educational materials or guidelines so that nurse educators can use critical reflection in nursing education.
In this pilot study, the program was found to be effective in improving critical thinking disposition and teaching efficacy. The results show that the program can enhance the critical thinking disposition of nurse educators and help them develop teaching competency by critically reflecting on their educational experiences as instructors [ 35 , 36 ]. Therefore, various educational programs and training systems related to critical reflection are required [ 37 ]. However, many medical institutions find it difficult to provide sufficient educational support to nurses because of limited costs, time, and physical space [ 38 ]. Online real-time lectures and case-based discussions of the developed program can be useful alternatives to overcome barriers to nursing education support. Additionally, more effective educational content and platforms using e-learning can be developed based on the results of this study.
In this study, the critical reflection competency program for clinical nurse educators was developed and conducted. The program was an educational intervention to improve the critical reflection competency of clinical nurse educators in real time online. Several limitations must be considered when interpreting the present findings. The developed program did not affect nursing reflection competencies. Further, the post-test was conducted shortly after program completion. Therefore, there may be limitations to evaluating whether the developed program improves the quality of nursing education. In addition, the participants in this study were allocated regardless of their hospital’s characteristics. Considering variables such as the size of the hospitals, the number of new nurses, and the number of participants per hospital, it is necessary to assign nurse educators the intervention and control groups and to verify the effects of the program. Future studies should consider improving the study design to measure the long-term effects of the program and randomize the participants.
The effects of the program on critical thinking disposition, nursing reflection competency, and teaching efficacy were assessed. The results showed that the program was effective in improving the critical thinking disposition and teaching efficacy of nurse educators. However, there was no significant difference in nursing reflection competency, but it may vary depending on the methods or time of using critical reflection in nursing education. Therefore, it is necessary to provide the critical reflection utilization strategies that can be used by clinical nurse educators in the clinical settings. In addition, further research, such as evaluating the reflective practice of new nurses trained by clinical nurse educators, is needed. This suggests that the critical reflection competency program should be expanded in the future for nurse educators. It is necessary to develop e-learning content and educational platforms to expand the program, and it should be possible to share the experience of critical reflection in various forms. Also, sufficient support for competency improvement of nurse educators is needed to effectively use critical reflection in nursing education. Nursing leaders in hospital and healthcare settings should recognize the importance of using critical reflection in clinical practice and improving the competency of clinical nursing educators who educate new nurses, and make efforts to improve the quality of nursing education through support for these. Lastly, based on the results of this study, we recommend further longitudinal and randomized studies to evaluate additional effects of the program.
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Kim YH, Min J, Kim SH, Shin S. Effects of a work-based critical reflection program for novice nurses. BMC Med Educ. 2018;18:1–6. https://doi.org/10.1186/s12909-018-1135-0 .
Article Google Scholar
Alfaro-LeFevre R. Critical thinking in nursing: a practical approach. Philadelphia, PA: W.B. Saunders; 1995.
Google Scholar
Do J, Shin S, Lee I, Jung Y, Hong E, Lee MS. Qualitative content analysis on critical reflection of clinical nurses. J Qual Res. 2021;22:86–96. https://doi.org/10.22284/qr.2021.22.86 .
Burrell LA. Integrating critical thinking strategies into nursing curricula. Teach Learn Nurs. 2014;9:53–8. https://doi.org/10.1016/j.teln.2013.12.005 .
Lee M, Jang K. Reflection-related research in korean nursing: a literature review. J Korean Acad Nurs Adm. 2019;25:83–96. https://doi.org/10.11111/jkana.2019.25.2 .
Cox K. Planning bedside teaching. Med J Aust. 1993;158:280–2. https://doi.org/10.5694/j.1326-5377.1993.tb137586.x .
Article CAS PubMed Google Scholar
Klaeson K, Berglund M, Gustavsson S. The character of nursing students’ critical reflection at the end of their education. J Nurs Educ Pract. 2017;7:55–61. https://doi.org/10.5430/jnep.v7n5p55 .
Pangh B, Jouybari L, Vakili MA, Sanagoo A, Torik A. The effect of reflection on nurse-patient communication skills in emergency medical centers. J Caring Sci. 2019;8:75–81. https://doi.org/10.15171/jcs.2019.011 .
Article PubMed PubMed Central Google Scholar
Liu K, Ball AF. Critical reflection and generativity: toward a framework of transformative teacher education for diverse learners. Rev Res Educ. 2019;43:68–105. https://doi.org/10.3102/0091732X18822806 .
Shin S, Kim SH. Experience of novice nurses participating in critical reflection program. J Qual Res. 2019;20:60–7. https://doi.org/10.22284/qr.2018.20.1.60 .
Lee M, Jang K. The significance and application of reflective practice in nursing practice. J Nurs Health Issues. 2018;23:1–8.
Monagle JL, Lasater K, Stoyles S, Dieckmann N. New graduate nurse experiences in clinical judgment: what academic and practice educators need to know. Nurs Educ Pers. 2018;39:201–7. https://doi.org/10.1097/01.NEP.0000000000000336 .
Bull R, Shearer T, Youl L, Campbell S. Enhancing graduate nurse transition: report of the evaluation of the clinical honors program. J Cont Educ Nurs. 2018;49:348–55. https://doi.org/10.3928/00220124-20180718-05 .
Cadmus E, Salmond SW, Hassler LJ, Black K, Bohnarczyk N. Creating a long-term care new nurse residency model. J Cont Educ Nurs. 2016;47:234–40. https://doi.org/10.3928/00220124-20160419-10 .
Johansson A, Berglund M, Kjellsdotter A. Clinical nursing introduction program for new graduate nurses in Sweden: study protocol for a prospective longitudinal cohort study. BMJ open. 2021;11:e042385. https://doi.org/10.1136/bmjopen-2020-042385 .
Salminen L, Minna S, Sanna K, Jouko K, Helena LK. The competence and the cooperation of nurse educators. Nurse Educ Today., 2013;33:1376–81. https://doi.org/10.1016/j.nedt.2012.09.008 .
Zlatanovic T, Havnes A, Mausethagen S. A research review of nurse teachers’ competencies. Vocations Learn. 2017;10:201 − 33. https://doi.org/10.1007/s12186-016-9169-0 .
Shinners JS, Franqueiro T. Preceptor skills and characteristics: considerations for preceptor education. J Cont Educ Nurs. 2015;46:233–6. https://doi.org/10.3928/00220124-20150420-04 .
Sheppard-Law S, Curtis S, Bancroft J, Smith W, Fernandez R. Novice clinical nurse educator’s experience of a self-directed learning, education and mentoring program: a qualitative study. Contemp Nurs. 2018;54:208–19. https://doi.org/10.1080/10376178.2018.1482222 .
Kang HJ, Bang KS. Development and evaluation of a self-reflection program for intensive care unit nurses who have experienced the death of pediatric patients. J Korean Acad Nurs. 2017;47:392-405. https://doi.org/10.4040/jkan.2017.47.3.392 .
Hayton A, Kang I, Wong R, Loo LK. Teaching medical students to reflect more deeply. Teach Learn Med. 2015;27:410-6. https://doi.org/10.1080/10401334.2015.1077124 .
Spampinato CM, Wittich CM, Beckman TJ, Cha SS, Pawlina W. Safe Harbor”: evaluation of a professionalism case discussion intervention for the gross anatomy course. Anat Sci Educ. 2014;7:191–8.
Article PubMed Google Scholar
Yoon J. Development of an instrument for the measurement of critical thinking disposition: In nursing[dissertation]. Seoul: Catholic University; 2004.
Lee H. Development and psychometric evaluation of nursing-reflection questionnaire [dissertation]. Seoul: Korea University; 2020.
Park I, Suh YO. Development of teaching efficacy scale to evaluate clinical nursing instructors. Korean J Adult Nurs. 2017;30:18–29. https://doi.org/10.7475/kjan.2018.30.1.18 .
Froneman K, du Plessis E, van Graan AC. Conceptual model for nurse educators to facilitate their presence in large class groups of nursing students through reflective practices: a theory synthesis. BMC Nurs. 2022;21:317. https://doi.org/10.1186/s12912-022-01095-7 .
Uygur J, Stuart E, De Paor M, Wallace E, Duffy S, O’Shea M, Smith S, Pawlikowska T. A best evidence in medical education systematic review to determine the most effective teaching methods that develop reflection in medical students. BEME Guide No 51 Med Teach. 2019;41:3–16. https://doi.org/10.1080/0142159X.2018.1505037 .
McEvoy M, Pollack S, Dyche L, Burton W. Near-peer role modeling: can fourth-year medical students, recognized for their humanism, enhance reflection among second-year students in a physical diagnosis course? Med Educ Online. 2016;21:31940. https://doi.org/10.3402/meo.v21.31940 .
Poulou M. Personal teaching efficacy and its sources: student teachers’ perceptions. Educ Psychol. 2007;27:191–218. https://doi.org/10.1080/01443410601066693 .
Klopfer BC, Piech EM. Characteristics of effective nurse educators. Sigma Theta Tau International: Leadership Connection 2016; 2016.
Dozier AL. An investigation of nursing faculty teacher efficacy in nursing schools in Georgia. ABNF J. 2019;30:50–7.
Kim EK, Shin S. Teaching efficacy of nurses in clinical practice education: a cross-sectional study. Nurse Educ Today. 2017;54:64–8. https://doi.org/10.1016/j.nedt.2017.04.017 .
Wu XV, Chi Y, Selvam UP, Devi MK, Wang W, Chan YS, Wee FC, Zhao S, Sehgal V, Ang NKE. A clinical teaching blended learning program to enhance registered nurse preceptors’ teaching competencies: Pretest and posttest study. J Med Internet Res. 2020;22:e18604. https://doi.org/10.2196/18604 .
Larsen R, Zahner SJ. The impact of web-delivered education on preceptor role self-efficacy and knowledge in public health nurses. Public Health Nurs. 2011;28:349–56. https://doi.org/10.1111/j.1525-1446.2010.00933.x .
Armstrong DK, Asselin ME. Supporting faculty during pedagogical change through reflective teaching practice: an innovative approach. Nurs Educ Pers. 2017;38:354–7. https://doi.org/10.1097/01.NEP.0000000000000153 .
Raymond C, Profetto-McGrath J, Myrick F, Strean WB. Balancing the seen and unseen: nurse educator as role model for critical thinking. Nurse Educ Prac. 2018;31:41–7. https://doi.org/10.1016/j.nepr.2018.04.010 .
Parrish DR, Crookes K. Designing and implementing reflective practice programs–key principles and considerations. Nurse Educ Prac. 2014;14:265–70. https://doi.org/10.1016/j.nepr.2013.08.002 .
Glogowska M, Young P, Lockyer L, Moule P. How ‘blended’ is blended learning?: students’ perceptions of issues around the integration of online and face-to-face learning in a continuing professional development (CPD) health care context. Nurse Educ Today. 2011;31:887–91. https://doi.org/10.1016/j.nedt.2011.02.003 .
Download references
Acknowledgements
Not applicable.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1F1A1057096).
Author information
Authors and affiliations.
College of Nursing, Ewha Womans University, 52 Ewhayeodae-gil, Seodaemun-gu, 03760, Seoul, Republic of Korea
Sujin Shin & Eunmin Hong
Department of Nursing, Dongnam Health University, 50, Cheoncheon-ro 74beon-gil, Jangan-gu, Suwon-si, Gyeonggi-do, Republic of Korea
Inyoung Lee
College of Nursing, Catholic University of Pusan, 57 Oryundae-ro, Geumjeong-gu, 46252, Busan, Republic of Korea
Jeonghyun Kim
Department of Nursing, Nursing Administration Education Team Leader, Catholic University of Korea Bucheon ST. Mary’s Hospital, 327, Sosa-ro, 14647, Bucheon-si, Gyeonggi-do, Republic of Korea
Eunyoung Oh
You can also search for this author in PubMed Google Scholar
Contributions
SS: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Project administration. IL: Conceptualization, Methodology, Formal analysis, Validation, Writing – review & editing. JK: Conceptualization, Methodology, Formal analysis, Validation, Writing – review & editing. EO: Data curation, Validation, Writing – review & editing. EH: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Visualization.
Corresponding author
Correspondence to Eunmin Hong .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board (IRB) of Ewha Womans University (IRB no. ewha-202105-0022-02). The need of written informed consent was exempted by IRB of Ewha Womans University. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shin, S., Lee, I., Kim, J. et al. Effectiveness of a critical reflection competency program for clinical nurse educators: a pilot study. BMC Nurs 22 , 69 (2023). https://doi.org/10.1186/s12912-023-01236-6
Download citation
Received : 12 December 2022
Accepted : 07 March 2023
Published : 16 March 2023
DOI : https://doi.org/10.1186/s12912-023-01236-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Education professional
- Nursing education research
- Program evaluation
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Critical self-reflection for nurse educators: Now more than ever!
Affiliation.
- 1 Malta College of Arts, Science and Technology (MCAST), Institute of Applied Sciences Corradino Hill, Paola, PLA9032 Malta.
- PMID: 33013247
- PMCID: PMC7522740
- DOI: 10.1016/j.teln.2020.09.001
The dynamic healthcare world and increased demands on nurses call for a parallel shift in nursing education that is optimally geared toward effectiveness. Just as student nurses are taught to reflect on their practice to effectively meet clients' needs, educators also need to be well versed in self-reflection to enhance their teaching methods. Self-reflection is the deliberate consideration of experiences, which when guided by the literature helps an individual gain insight and improve practice. Educators should not only opt for personal reflection but should also seek the views of their students and peers. Self-reflection becomes critical when it goes beyond mere reflection, questioning teaching assumptions, and addressing their social and political context. Given the remarked benefits of using self-reflection in education, and the current COVID-19 global repercussions which have urged faculties to try alternative methods of teaching, a concise guide to self-reflection is hereby provided for use by nurse educators.
Keywords: COVID-19; Nursing education; Nursing faculty; Reflection.
© 2020 Organization for Associate Degree Nursing. Published by Elsevier Inc. All rights reserved.
Why Self-Reflection Is Critical In Nursing Education—Drive Lifelong Learning and Future Success
As future healthcare providers, nursing students not only need to master a rigorous curriculum and complex concepts but also develop a wide range of clinical skills and knowledge to deliver high-quality patient care. Several characteristics have been identified as key to optimizing nursing care, including self-motivation, positive workplace culture, and a strong enabling leadership. 1
Another skill that has emerged as critical in nursing education is self-reflection, which involves accurately identifying and analyzing one’s thoughts, actions, and feelings, requiring cognitive activities such as description, critical analysis, evaluation, and planning. When applied to practice, it improves nurses’ self-efficacy and work engagement 2 —values that enable high-quality patient care. One study found significant and positive correlations between these three qualities.
For more ways to help your nursing students develop self-reflection, download our Educator Guide: How Educators Can Foster Self-Reflection in Healthcare Learning—and Empower Learners to Become Successful Practitioners

The connection between self-reflection, self-efficacy, and work engagement
Using a stratified random sampling method and inclusion criteria that included holding a bachelor’s degree in nursing and clinical working experience, a total of 240 nurses from seven hospitals were selected for the study. 3 Data were collected via three questionnaires: Groningen Reflection Ability Scale (GRAS), Sherer’s General Self-Efficacy Scale (SGSES), and Utrecht Work Engagement Scale (UWES).
Overall, the nurses’ total reflection scores were found to correlate positively and significantly with their work engagement and self-efficacy levels.
Does this suggest that nursing students should be encouraged to cultivate this practice from the start of their program and in clinical settings? Let’s take a closer look at key findings from the study.
Self-reflection
The nurses in the study exhibited a robust reflective practice, as indicated by a relatively high level of reflection—the mean score was 86.51 out of 115. Notably, there was a statistically significant difference in the reflection scores of nurses working in the emergency department (ED) compared to nurses in other departments; ED nurses had a higher mean score.
Why this is important
Self-reflection has an essential role in nursing education and practice: it facilitates the learning of clinical nurses, boosts the quality of care provided, and encourages nurses to search for and discover solutions to difficult situations. Through self-reflection, nurses gain new experiences and insights from both clinical and educational settings. This process helps them develop a sense of ownership over the acquired knowledge, enhancing their expertise and clinical decision-making. 4
Self-efficacy
The nurses demonstrated a high level of self-efficacy—60.89 out of 85—and similar to self-reflection, ED nurses had a higher mean score than their counterparts in other departments. Additionally, there was a statistically significant correlation between self-efficacy with age and years of work experience, underscoring the value of experience in building confidence and capability in clinical practice.
The self-efficacy theory is based on the premise that individuals’ beliefs about their abilities positively influence their actions and activities. Nurses with high self-efficacy are more motivated, provide higher quality patient care, and can more effectively overcome challenges due to their enhanced problem-solving skills. When faced with difficulties, these nurses focus on their abilities to find solutions and navigate situations successfully.
Work engagement
The study indicated that the mean work engagement score among nurses was 3.39 out of 6. Engaged nurses are more likely to experience job satisfaction, which can lead to higher retention rates and improved patient care outcomes.
Work engagement refers to an individual’s commitment to their organization or employer and has a positive effect on both employee performance and organizational outcomes. Key variables influenced by work engagement include job satisfaction, organizational commitment, and work performance, and they encompass feelings of vigor and identification with work activities.
Pearson correlation matrix showing the correlation between nurses’ reflection, self-efficacy, and work engagement level
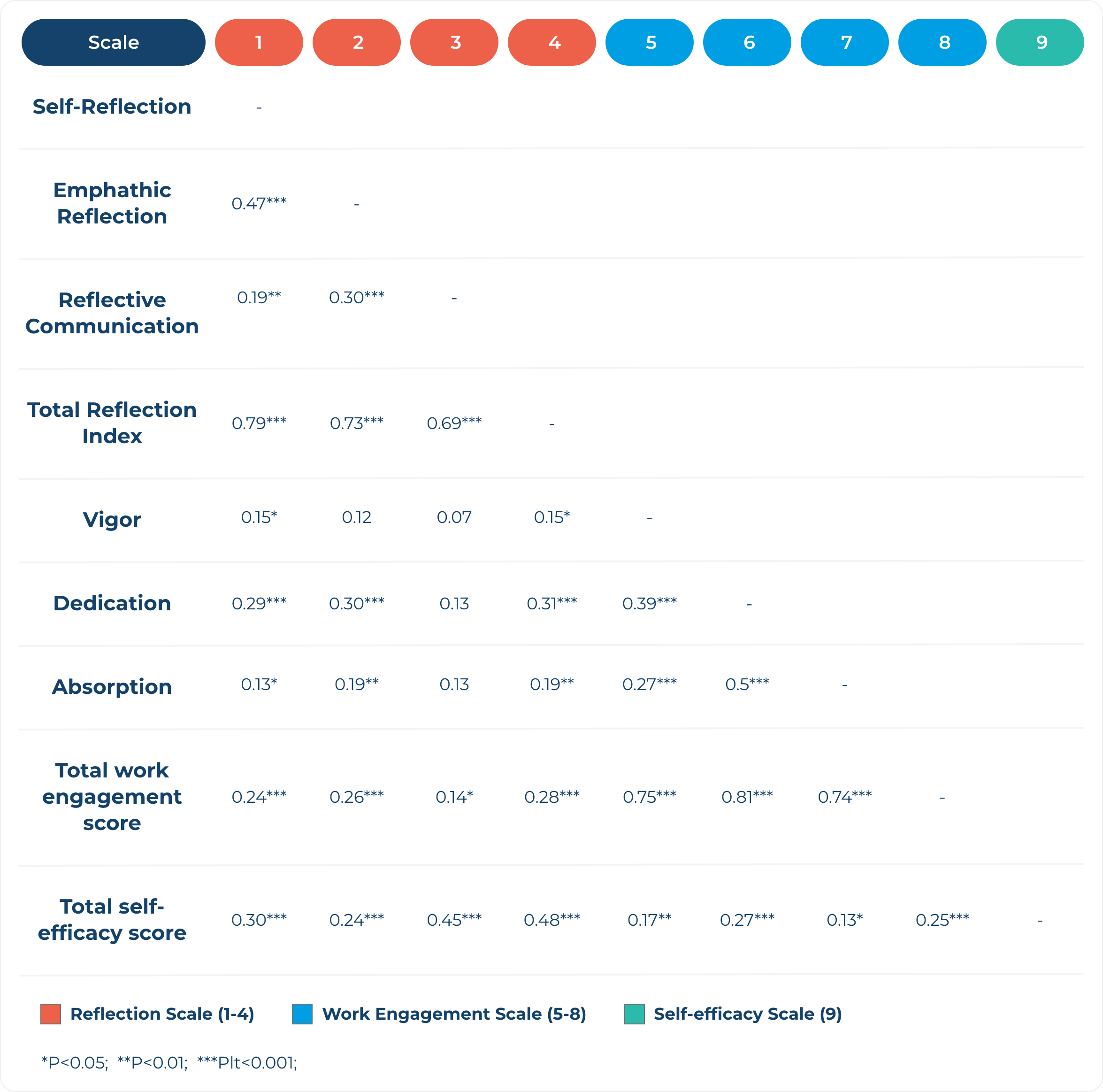
The results of the study indicated a positive and significant relationship between self-reflection, self-efficacy, and work engagement among nurses: the mean score for each rose in tandem with the others. This is consistent with another study that reported high self-reflection scores corresponded with high self-efficacy scores 5 while a study on ICU (intensive care unit) nurses 6 showed a significant correlation between self-reflection and work engagement.
What Does This Mean for Nursing Education?
Self-reflection brings about many positive consequences for nurses, including supporting the development of lifelong learning habits for optimum personal and professional development; enabling them to deliver better quality of patient care and support; and boosting knowledge, attitude, and practices regarding ethical codes, leading to improved clinical competency.
Thus, self-reflection should be integrated into nursing education so that students can start building these qualities from day one of nursing school and sharpen them across their journey toward licensure and in future practice.
Programs and faculty can help nursing students cultivate self-reflection by pairing learning science-based resources such as Picmonic’s 1,300+ audio-visual mnemonic video lessons and TrueLearn’s NCLEX-style critical thinking questions with self-reflection practices to:
- Get immediate, real-time feedback on performance and comprehension
- Interact meaningfully with the content (active learning), improve long-term retention and ease of recall
- Identify learning strengths and weaknesses, pinpoint areas for improvement
- Track and measure learning progress and exam readiness longitudinally
- Adjust/tailor teaching/study methods for the most effective, efficient learning
Learn more about a partnership with TrueLearn and Picmonic here.
Help your nursing students achieve optimal exam performance and outcomes, read and share this blog with them and encourage them to utilize our free Post-Assessment Self-Reflection Questionnaire!
1 King R, Taylor B, Talpur A, et al. Factors that optimise the impact of continuing professional development in nursing: A rapid evidence review. Nurse Educ Today. 2021;98(104652):104652. doi:10.1016/j.nedt.2020.104652
2 Tbzmed.ac.ir. Accessed July 24, 2024. https://jcs.tbzmed.ac.ir/Article/jcs-31920
3 Zarrin L, Ghafourifard M, Sheikhalipour Z. Relationship between nurses reflection, self-efficacy and work engagement: A multicenter study. J Caring Sci. 2023;12(3):155-162. doi:10.34172/jcs.2023.31920
4 Razieh S, Somayeh G, Fariba H. Effects of reflection on clinical decision-making of intensive care unit nurses. Nurse Educ Today. 2018;66:10-14. doi:10.1016/j.nedt.2018.03.009
5 Sundgren MKM, Dawber C, Millear PM, Medoro L. Reflective practice groups and nurse professional quality of life. Aust J Adv Nurs. 2021;38(4). doi:10.37464/2020.384.355
6 Lawrence LA. Work engagement, moral distress, education level, and critical reflective practice in intensive care nurses: Critical reflective practice in intensive care nurses. Nurs Forum. 2011;46(4):256-268. doi:10.1111/j.1744-6198.2011.00237.x
Related Content

Empower Nurse Educators to Fight Nursing Student Attrition a...

Fighting Nurse Attrition with Science-Backed Audio-Visual Mn...

Five Ways Picmonic Benefits Nursing Students and Faculty
Subscribe to TrueLearn's Newsletter
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Effectiveness of a critical reflection competency program for clinical nurse educators: a pilot study
Inyoung lee, jeonghyun kim, eunyoung oh, eunmin hong.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Received 2022 Dec 12; Accepted 2023 Mar 7; Collection date 2023.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Critical reflection is an effective learning strategy that enhances clinical nurses’ reflective practice and professionalism. Therefore, training programs for nurse educators should be implemented so that critical reflection can be applied to nursing education. This study aimed to investigate the effects of a critical reflection competency program for clinical nurse educators on improving critical thinking disposition, nursing reflection competency, and teaching efficacy.
A pilot study was conducted using a pre- and post-test control-group design. Participants were clinical nurse educators recruited using a convenience sampling method. The program was conducted once a week for 90 min, with a total of four sessions. The effectiveness of the developed program was verified by analyzing pre- and post-test results of 26 participants in the intervention group and 27 participants in the control group, respectively. The chi-square test, independent t-test, Mann-Whitney U test, and analysis of covariance with age as a covariate were conducted.
The critical thinking disposition and teaching efficacy of the intervention group improved after the program, and the differences between the control and intervention groups were statistically significant (F = 14.751, p < 0.001; F = 11.047, p < 0.001). There was no significant difference in the change in nursing reflection competency between the two groups (F = 2.674, p = 0.108).
The critical reflection competency program was effective in improving the critical thinking disposition and teaching efficacy of nurse educators. Therefore, it is necessary to implement the developed program for nurse educators to effectively utilize critical reflection in nursing education.
Keywords: Education professional, Nurses, Nursing education research, Program evaluation
The critical thinking of clinical nurses is essential for identifying the needs of patients and providing safe care through prompt and accurate judgment [ 1 – 3 ]. Critical thinking can be practiced through critical reflection [ 4 ], a dynamic process in which nurses reflect on their nursing behavior to improve their perspective on a situation and change future nursing practices in a desirable direction [ 5 ]. Through critical reflection, nurses grasp the contextual meaning of a situation and reconstruct their experiences to apply their learning in practice, thereby identifying the meaning of nursing [ 3 ]. In other words, critical reflection can help nurses convert their experiences into practical knowledge [ 6 ]. Thus, critical reflection may be an effective learning strategy linking theory and practice in clinical nursing education [ 7 ].
Studies have reported that critical reflection is effective in improving nurses’ reflective practices and professionalism. Teaching methods that use critical reflection can improve nurses’ knowledge, communication skills, and critical thinking abilities [ 1 , 8 , 9 ]. These methods can be effective in improving clinical judgment and problem-solving abilities by providing new nurses with opportunities to apply their theoretical knowledge in clinical practice [ 10 , 11 ]. In addition, critical reflection has positive effects on the professionalism of new graduate nurses and reduces reality shock during the transition from university to clinical practice [ 12 ]. These advantages have led to the increasing application of critical reflection in training programs for new graduate nurses, including nursing residency programs [ 13 – 15 ].
In order to facilitate new nurses’ reflective thinking and practice by clinical nurse educators, educators must be trained to strengthen their critical thinking disposition, nursing reflection, and teaching efficacy competency. Educators help new nurses adapt and develop their expertise in clinical settings [ 16 , 17 ]. Moreover, continuing education for nurses to improve their teaching competency relates to the satisfaction of learners and nurse educators, which improves the quality of clinical nursing education [ 18 ]. Therefore, opportunities for nurse educators to develop teaching competency for critical reflection in education should be provided [ 19 ] and educational support for nurse educators to improve critical reflection competency is needed.
However, although there have been studies that have evaluated the effectiveness of the educational interventions concerning critical reflection to new nurses, few studies have been conducted on educational interventions on the critical reflection competencies of clinical nurse educators in charge of educating new nurses. Therefore, this study aimed to investigate the effects of a critical reflection competency program for clinical nurse educators on improving critical thinking disposition, nursing reflection competency, and teaching efficacy.
Study design
A pilot study was conducted with a pre- and post-test control group design to investigate the effects of the critical reflection competency program on the critical thinking disposition, nursing reflection competency, and teaching efficacy of nurse educators. The conceptual framework in this study was proposed that the critical reflection competency program will improve critical thinking disposition, nursing reflection, and teaching efficacy of clinical nurse educators [Fig. 1 ].
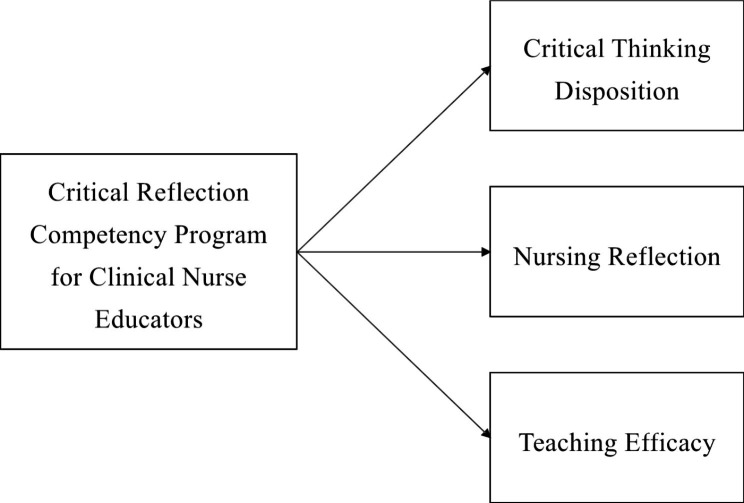
Conceptual Framework
Participants were clinical nurse educators in hospitals who were recruited using a convenience sampling method. Nurse educators were eligible to participate if they had dedicated nursing education in a clinical setting. They dedicated to nursing education focused on staff development of current nurses, especially the education for new nurses. They also included those who completed all four sessions of the program and participated in the data collection before and after the program. A recruitment document was sent to hospitals to recruit the participants, hospitals were selected with concerning role of clinical nurse educators. Participants were recruited from two hospitals of different sizes and the number of participants differed for each hospital, and they were allocated according to the order of registration.
The sample size required for the analysis was calculated using the G* Power 3.1.9.4. program with an effect size of 0.80, a significance level of 0.05, and a power of 0.80, following the literature [ 20 ]. By applying a self-reflection program for intensive care unit nurses [ 20 ], we calculated the effect size as large. Both the intervention and control groups required 26 participants. Considering a dropout rate of 20%, a total of 63 participants, including 32 in the intervention group and 31 in the control group, were recruited. From the intervention group, six participants who participated in the pre-test and completed all programs, but did not participate in the post-test, were excluded. In the control group, four participants who participated in the pre-test but not in the post-test were excluded. Thus, 26 and 27 participants in the intervention and control groups, respectively, were included in the final analysis [Fig. 2 ]. The pre-test for both groups was conducted in May 2021. Post-tests for the two groups were performed four weeks after the pre-test.
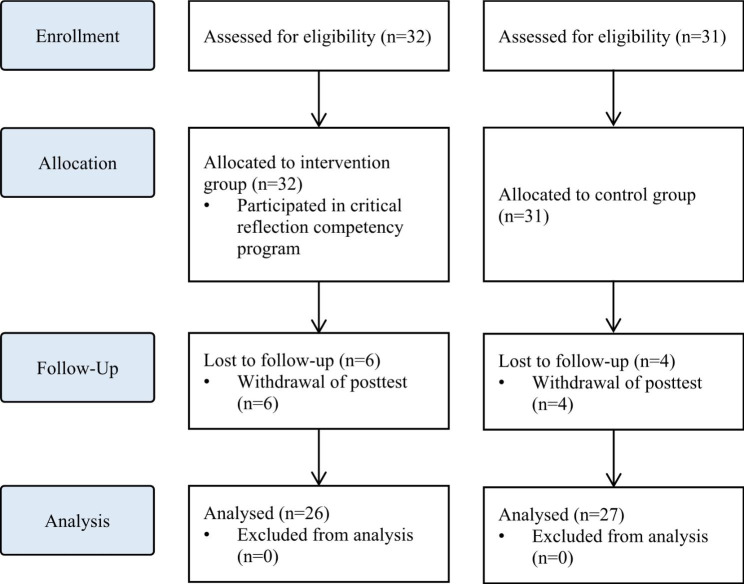
Flowchart of the study
Intervention
The intervention was developed and delivered by the first author, who has more than 15 years of teaching experience in nursing education, including critical reflection. The intervention was conducted between May 2021 and June 2021. Following previous studies that applied critical reflection in medical education [ 21 , 22 ], the intervention was conducted once a week for 90 min, with a total of four sessions. Owing to COVID-19, real-time online sessions were used to minimize contact between participants working in medical institutions. Every week before the sessions, the contents of the session, schedule, and Uniform Resource Locator (URL) were sent to participants via e-mail.
The intervention consisted of the following three steps in four sessions: (1) understanding critical reflection, (2) strategies to use critical reflection, and (3) practical uses of critical reflection [Fig. 3 ]. Synchronous online lectures were conducted in the first and second sessions. The contents of the first session included understanding of critical reflection and the clinical judgment process through critical reflection. Based on the content of the first session, the second outlined educational strategies using critical reflection in nursing education and the direction of critical reflection. In the third and fourth sessions, clinical nurses with experience of critically reflecting on themselves were invited as guest speakers to share their experiences and facilitate online discussions. Online discussions were also conducted in real time, and feedback from guest speakers and the author was immediately provided.
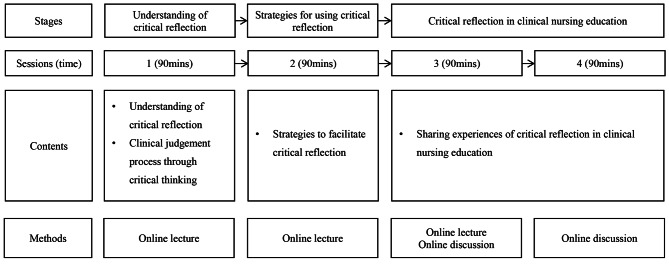
Critical reflection program for clinical nurse educators
Online self-report surveys were conducted before and after the program to assess the program’s effects. In both pre- and post-tests, critical thinking disposition, nursing reflection competency, and teaching efficacy were assessed, as well as information about participants, such as gender, age, experience in nursing education, and the type of institution and the number of beds they affiliated with.
Critical thinking disposition was measured using Yoon’s Critical Thinking Disposition Scale [ 23 ]. This scale comprises 27 items: 5 on “intellectual eagerness/curiosity,” 4 on “prudence,” 4 on “self-confidence,” 3 on “systematicity,” 4 on “intellectual fairness,” 4 on “healthy skepticism,” and 3 on “objectivity.” The items were evaluated on a five-point Likert scale (one point for “strongly disagree” to five points for “strongly agree”); a higher score indicated greater critical thinking disposition. The scale has good reliability as evidenced by a Cronbach’s alpha of 0.84 at the time of the development versus the reliability of the scale in this study was Cronbach’s alpha of 0.78.
Nursing reflection competency was assessed using the Nursing-Reflection Questionnaire, developed by Lee et al. [ 24 ]. This scale comprises four factors with 15 items, including 6 items on “review and analysis nursing behavior,” 5 on “development-oriented deliberative engagement,” 2 on “objective self-awareness,” and 2 on “contemplation of behavioral change.” Each item was evaluated on a five-point Likert scale (one point for “strongly disagree” to five points for “strongly agree”), with a higher score indicating greater nursing reflection competency. The scale has good reliability as evidenced by a Cronbach’s alpha of 0.86 at the time of the development versus the reliability of the scale in this study was Cronbach’s alpha of 0.82.
Teaching efficacy was evaluated using the Teaching Efficacy Scale developed by Park and Suh [ 25 ] to evaluate clinical nursing instructors. This scale consisted of six sub-factors with 42 items, including 12 items on “student instruction,” 9 on “teaching improvement,” 7 on “application of teaching and learning,” 7 on “interpersonal relationship and communication,” 4 on “clinical judgment,” and 3 on “clinical skill instruction.” Each item was evaluated on a five-point Likert scale (one point for “strongly disagree” to five points for “strongly agree”), with a higher score indicating greater teaching efficacy. The scale has good reliability as evidenced by a Cronbach’s alpha of 0.97 at the time of the development versus the reliability of the scale in this study was Cronbach’s alpha of 0.93.

Ethical considerations
This study was approved by the Institutional Review Board (IRB) of Ewha Womans University (IRB no. ewha-202105-0022-02). The need of written informed consent was exempted by IRB of Ewha Womans University. All methods were performed in accordance with the relevant guidelines and regulations. A description of the study, including its purpose, methods, and procedures, was posted on an online pre-test survey. Only those participants who agreed to participate were allowed to complete the questionnaire. The participants were also informed that they could withdraw from the study at any time and that the data of withdrawn participants would not be included in the final analysis. After the survey was completed, a mobile gift voucher was provided to those who agreed to provide their mobile phone number. Data were collected by researchers who did not participate in the program.
Data analysis
The collected data were analyzed using SPSS for Windows (version 28.0). Non-normally distributed data were analyzed using non-parametric tests. Descriptive statistics were used to calculate the frequency, percentage, mean, and standard deviation of participants’ general and institutional characteristics. Chi-square, independent t-, and Mann-Whitney U tests were conducted to test the homogeneity of the general characteristics and pre-test scores. The Shapiro-Wilk test was conducted to test the normality of the data. To test the difference between the pre- and post-tests for each group, analysis of covariance (ANCOVA) was used. As there was a significant difference in age between the intervention and control groups, an ANCOVA with age as a covariate was conducted for the difference in changes in test scores between the pre- and post-test.
Homogeneity test of general characteristics and dependent variables
All participants were female, with a mean nursing education experience of 27 and 23 months in the intervention and control groups, respectively. The homogeneity test of general and institutional characteristics, such as gender, nursing education experience, affiliated institution types, and the number of beds, were not statistically significant. However, the age differed significantly between the two groups. In the test for homogeneity of the pre-intervention scores, there were no significant differences in critical thinking disposition, nursing reflection competency, or teaching efficacy between the two groups, suggesting homogeneity of the dependent variables between the groups [Table 1 ].
Homogeneity test on general characteristics and dependent variables (N = 53)
* Independent t-test; ** Chi-square test; *** Mann-Whitney U test; Exp.=experimental group; Cont.=control group
Effects of critical reflection competency program
The effects of the critical reflection competency program are shown in Table 2 .
Effects of critical reflection competency program (N = 53)
* Ranked ANCOVA; Exp.=experimental group; Cont.=control group; LSM = least mean square
In the post-intervention phase, scores of critical thinking disposition, nursing reflection competency, and teaching efficacy all improved compared to the pre-intervention phase, and were higher in the experimental group than in the control group. The critical thinking disposition scores before and after the intervention were 3.61 ± 0.26 vs. 3.87 ± 0.04 in the intervention group and 3.76 ± 0.21 vs. 3.77 ± 0.04 in the control group, respectively. The nursing reflection competency scores before and after the intervention were 57.00 ± 3.42 vs. 60.86 ± 0.95 in the intervention group and 59.63 ± 5.24 vs. 59.04 ± 0.89 in the control group. The teaching efficacy scores before and after the intervention were 157.04 ± 10.60 vs. 171.98 ± 2.54 in the intervention group and 161.59 ± 14.77 vs. 160.48 ± 2.46 in the control group.
Age, which was significantly different between the intervention and control groups, was treated as a covariate to conduct the ANCOVA. The changes in critical thinking disposition (F = 14.751, p < 0.001) and teaching efficacy (F = 11.047, p < 0.001) scores were significantly different between the two groups. However, there was no significant difference in the change in the nursing reflection competency (F = 2.674, p = 0.108) score between the two groups.
Reflective practice is crucial to clinical nurses’ professionalism. Reflective practice enables positive learning experiences through deep and meaningful learning, and is essential for integrating theory and practice. It also enables nurses to implement what they have learned into practice, understand their expertise, and develop clinical competencies [ 26 ]. In this respect, it is important for clinical nursing educators to have critical reflection competencies and promote experiential learning among new nurses. In this study, a critical reflection competency program was developed to enhance clinical nurse educators’ critical thinking and teaching competency.
This program was effective in improving critical thinking disposition. In interventions for critical reflection, various aspects, including the introduction of critical reflection and guidelines to promote critical reflection, such as small group discussions and feedback, can be considered [ 27 ]. The program reflected these aspects and helped improve participants’ critical thinking disposition. In the third and fourth sessions, synchronous discussions on sharing experiences of critical reflection were effective. This is consistent with previous studies in which discussions improved reflective competencies [ 21 , 28 ]. Therefore, sharing experiences in the discussion section should be a key element of future educational interventions for critical reflection competency.
Furthermore, the program was effective in improving teaching efficacy. Teaching efficacy is the instructor’s belief in one’s own ability to organize and implement teaching [ 29 ], and is closely related to age, clinical experience, educational experience, professional development, and teaching competency [ 30 – 32 ]. Nurses who are more clearly aware of their roles as instructors tend to exhibit higher confidence in their teaching abilities [ 33 , 34 ]. That is, the participants in this study were clearly aware of their roles and developed confidence by sharing their educational experiences about critical reflection.
However, the program did not have a significant effect on nursing reflection competencies. In a previous study [ 10 ], reflective practitioners (RPs) received four weeks of critical reflection training and trained new nurses for six months. During training, new nurses wrote critical reflective journals and RPs provided feedback and shared their experiences. In this study, it seems that the methods and frequency of using critical reflection in nursing education varied for each participant, resulting in insignificant results for nursing reflection competency. It is necessary to provide educational materials or guidelines so that nurse educators can use critical reflection in nursing education.
In this pilot study, the program was found to be effective in improving critical thinking disposition and teaching efficacy. The results show that the program can enhance the critical thinking disposition of nurse educators and help them develop teaching competency by critically reflecting on their educational experiences as instructors [ 35 , 36 ]. Therefore, various educational programs and training systems related to critical reflection are required [ 37 ]. However, many medical institutions find it difficult to provide sufficient educational support to nurses because of limited costs, time, and physical space [ 38 ]. Online real-time lectures and case-based discussions of the developed program can be useful alternatives to overcome barriers to nursing education support. Additionally, more effective educational content and platforms using e-learning can be developed based on the results of this study.
In this study, the critical reflection competency program for clinical nurse educators was developed and conducted. The program was an educational intervention to improve the critical reflection competency of clinical nurse educators in real time online. Several limitations must be considered when interpreting the present findings. The developed program did not affect nursing reflection competencies. Further, the post-test was conducted shortly after program completion. Therefore, there may be limitations to evaluating whether the developed program improves the quality of nursing education. In addition, the participants in this study were allocated regardless of their hospital’s characteristics. Considering variables such as the size of the hospitals, the number of new nurses, and the number of participants per hospital, it is necessary to assign nurse educators the intervention and control groups and to verify the effects of the program. Future studies should consider improving the study design to measure the long-term effects of the program and randomize the participants.
The effects of the program on critical thinking disposition, nursing reflection competency, and teaching efficacy were assessed. The results showed that the program was effective in improving the critical thinking disposition and teaching efficacy of nurse educators. However, there was no significant difference in nursing reflection competency, but it may vary depending on the methods or time of using critical reflection in nursing education. Therefore, it is necessary to provide the critical reflection utilization strategies that can be used by clinical nurse educators in the clinical settings. In addition, further research, such as evaluating the reflective practice of new nurses trained by clinical nurse educators, is needed. This suggests that the critical reflection competency program should be expanded in the future for nurse educators. It is necessary to develop e-learning content and educational platforms to expand the program, and it should be possible to share the experience of critical reflection in various forms. Also, sufficient support for competency improvement of nurse educators is needed to effectively use critical reflection in nursing education. Nursing leaders in hospital and healthcare settings should recognize the importance of using critical reflection in clinical practice and improving the competency of clinical nursing educators who educate new nurses, and make efforts to improve the quality of nursing education through support for these. Lastly, based on the results of this study, we recommend further longitudinal and randomized studies to evaluate additional effects of the program.
Acknowledgements
Not applicable.
Authors’ contributions
SS: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Project administration. IL: Conceptualization, Methodology, Formal analysis, Validation, Writing – review & editing. JK: Conceptualization, Methodology, Formal analysis, Validation, Writing – review & editing. EO: Data curation, Validation, Writing – review & editing. EH: Conceptualization, Methodology, Formal analysis, Investigation, Data curation, Writing – original draft, Visualization.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2020R1F1A1057096).
Data availability
The datasets used or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate.
This study was approved by the Institutional Review Board (IRB) of Ewha Womans University (IRB no. ewha-202105-0022-02). The need of written informed consent was exempted by IRB of Ewha Womans University. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sujin Shin, Email: [email protected].
Inyoung Lee, Email: [email protected].
Jeonghyun Kim, Email: [email protected].
Eunyoung Oh, Email: [email protected].
Eunmin Hong, Email: [email protected].
- 1. Kim YH, Min J, Kim SH, Shin S. Effects of a work-based critical reflection program for novice nurses. BMC Med Educ. 2018;18:1–6. doi: 10.1186/s12909-018-1135-0. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Alfaro-LeFevre R. Critical thinking in nursing: a practical approach. Philadelphia, PA: W.B. Saunders; 1995. [ Google Scholar ]
- 3. Do J, Shin S, Lee I, Jung Y, Hong E, Lee MS. Qualitative content analysis on critical reflection of clinical nurses. J Qual Res. 2021;22:86–96. doi: 10.22284/qr.2021.22.86. [ DOI ] [ Google Scholar ]
- 4. Burrell LA. Integrating critical thinking strategies into nursing curricula. Teach Learn Nurs. 2014;9:53–8. doi: 10.1016/j.teln.2013.12.005. [ DOI ] [ Google Scholar ]
- 5. Lee M, Jang K. Reflection-related research in korean nursing: a literature review. J Korean Acad Nurs Adm. 2019;25:83–96. doi: 10.11111/jkana.2019.25.2. [ DOI ] [ Google Scholar ]
- 6. Cox K. Planning bedside teaching. Med J Aust. 1993;158:280–2. doi: 10.5694/j.1326-5377.1993.tb137586.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Klaeson K, Berglund M, Gustavsson S. The character of nursing students’ critical reflection at the end of their education. J Nurs Educ Pract. 2017;7:55–61. doi: 10.5430/jnep.v7n5p55. [ DOI ] [ Google Scholar ]
- 8. Pangh B, Jouybari L, Vakili MA, Sanagoo A, Torik A. The effect of reflection on nurse-patient communication skills in emergency medical centers. J Caring Sci. 2019;8:75–81. doi: 10.15171/jcs.2019.011. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Liu K, Ball AF. Critical reflection and generativity: toward a framework of transformative teacher education for diverse learners. Rev Res Educ. 2019;43:68–105. doi: 10.3102/0091732X18822806. [ DOI ] [ Google Scholar ]
- 10. Shin S, Kim SH. Experience of novice nurses participating in critical reflection program. J Qual Res. 2019;20:60–7. doi: 10.22284/qr.2018.20.1.60. [ DOI ] [ Google Scholar ]
- 11. Lee M, Jang K. The significance and application of reflective practice in nursing practice. J Nurs Health Issues. 2018;23:1–8. [ Google Scholar ]
- 12. Monagle JL, Lasater K, Stoyles S, Dieckmann N. New graduate nurse experiences in clinical judgment: what academic and practice educators need to know. Nurs Educ Pers. 2018;39:201–7. doi: 10.1097/01.NEP.0000000000000336. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Bull R, Shearer T, Youl L, Campbell S. Enhancing graduate nurse transition: report of the evaluation of the clinical honors program. J Cont Educ Nurs. 2018;49:348–55. doi: 10.3928/00220124-20180718-05. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Cadmus E, Salmond SW, Hassler LJ, Black K, Bohnarczyk N. Creating a long-term care new nurse residency model. J Cont Educ Nurs. 2016;47:234–40. doi: 10.3928/00220124-20160419-10. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Johansson A, Berglund M, Kjellsdotter A. Clinical nursing introduction program for new graduate nurses in Sweden: study protocol for a prospective longitudinal cohort study. BMJ open. 2021;11:e042385. doi: 10.1136/bmjopen-2020-042385. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Salminen L, Minna S, Sanna K, Jouko K, Helena LK. The competence and the cooperation of nurse educators. Nurse Educ Today., 2013;33:1376–81. 10.1016/j.nedt.2012.09.008. [ DOI ] [ PubMed ]
- 17. Zlatanovic T, Havnes A, Mausethagen S. A research review of nurse teachers’ competencies. Vocations Learn. 2017;10:201 − 33. 10.1007/s12186-016-9169-0.
- 18. Shinners JS, Franqueiro T. Preceptor skills and characteristics: considerations for preceptor education. J Cont Educ Nurs. 2015;46:233–6. doi: 10.3928/00220124-20150420-04. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Sheppard-Law S, Curtis S, Bancroft J, Smith W, Fernandez R. Novice clinical nurse educator’s experience of a self-directed learning, education and mentoring program: a qualitative study. Contemp Nurs. 2018;54:208–19. doi: 10.1080/10376178.2018.1482222. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Kang HJ, Bang KS. Development and evaluation of a self-reflection program for intensive care unit nurses who have experienced the death of pediatric patients. J Korean Acad Nurs. 2017;47:392-405. 10.4040/jkan.2017.47.3.392. [ DOI ] [ PubMed ]
- 21. Hayton A, Kang I, Wong R, Loo LK. Teaching medical students to reflect more deeply. Teach Learn Med. 2015;27:410-6. 10.1080/10401334.2015.1077124. [ DOI ] [ PubMed ]
- 22. Spampinato CM, Wittich CM, Beckman TJ, Cha SS, Pawlina W. Safe Harbor”: evaluation of a professionalism case discussion intervention for the gross anatomy course. Anat Sci Educ. 2014;7:191–8. doi: 10.1002/ase.1395. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Yoon J. Development of an instrument for the measurement of critical thinking disposition: In nursing[dissertation]. Seoul: Catholic University; 2004.
- 24. Lee H. Development and psychometric evaluation of nursing-reflection questionnaire [dissertation]. Seoul: Korea University; 2020.
- 25. Park I, Suh YO. Development of teaching efficacy scale to evaluate clinical nursing instructors. Korean J Adult Nurs. 2017;30:18–29. doi: 10.7475/kjan.2018.30.1.18. [ DOI ] [ Google Scholar ]
- 26. Froneman K, du Plessis E, van Graan AC. Conceptual model for nurse educators to facilitate their presence in large class groups of nursing students through reflective practices: a theory synthesis. BMC Nurs. 2022;21:317. doi: 10.1186/s12912-022-01095-7. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Uygur J, Stuart E, De Paor M, Wallace E, Duffy S, O’Shea M, Smith S, Pawlikowska T. A best evidence in medical education systematic review to determine the most effective teaching methods that develop reflection in medical students. BEME Guide No 51 Med Teach. 2019;41:3–16. doi: 10.1080/0142159X.2018.1505037. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. McEvoy M, Pollack S, Dyche L, Burton W. Near-peer role modeling: can fourth-year medical students, recognized for their humanism, enhance reflection among second-year students in a physical diagnosis course? Med Educ Online. 2016;21:31940. doi: 10.3402/meo.v21.31940. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Poulou M. Personal teaching efficacy and its sources: student teachers’ perceptions. Educ Psychol. 2007;27:191–218. doi: 10.1080/01443410601066693. [ DOI ] [ Google Scholar ]
- 30. Klopfer BC, Piech EM. Characteristics of effective nurse educators. Sigma Theta Tau International: Leadership Connection 2016; 2016.
- 31. Dozier AL. An investigation of nursing faculty teacher efficacy in nursing schools in Georgia. ABNF J. 2019;30:50–7. [ Google Scholar ]
- 32. Kim EK, Shin S. Teaching efficacy of nurses in clinical practice education: a cross-sectional study. Nurse Educ Today. 2017;54:64–8. doi: 10.1016/j.nedt.2017.04.017. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Wu XV, Chi Y, Selvam UP, Devi MK, Wang W, Chan YS, Wee FC, Zhao S, Sehgal V, Ang NKE. A clinical teaching blended learning program to enhance registered nurse preceptors’ teaching competencies: Pretest and posttest study. J Med Internet Res. 2020;22:e18604. doi: 10.2196/18604. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Larsen R, Zahner SJ. The impact of web-delivered education on preceptor role self-efficacy and knowledge in public health nurses. Public Health Nurs. 2011;28:349–56. doi: 10.1111/j.1525-1446.2010.00933.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Armstrong DK, Asselin ME. Supporting faculty during pedagogical change through reflective teaching practice: an innovative approach. Nurs Educ Pers. 2017;38:354–7. doi: 10.1097/01.NEP.0000000000000153. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Raymond C, Profetto-McGrath J, Myrick F, Strean WB. Balancing the seen and unseen: nurse educator as role model for critical thinking. Nurse Educ Prac. 2018;31:41–7. doi: 10.1016/j.nepr.2018.04.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Parrish DR, Crookes K. Designing and implementing reflective practice programs–key principles and considerations. Nurse Educ Prac. 2014;14:265–70. doi: 10.1016/j.nepr.2013.08.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Glogowska M, Young P, Lockyer L, Moule P. How ‘blended’ is blended learning?: students’ perceptions of issues around the integration of online and face-to-face learning in a continuing professional development (CPD) health care context. Nurse Educ Today. 2011;31:887–91. doi: 10.1016/j.nedt.2011.02.003. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
- View on publisher site
- PDF (1.5 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Learning Materials
- Business Studies
- Combined Science
- Computer Science
- Engineering
- English Literature
- Environmental Science
- Human Geography
- Macroeconomics
- Microeconomics
- Critical Reflection
Dive deep into the significant aspect of nursing - Critical Reflection. This comprehensive guide offers a thorough understanding of the concept and its importance in the field. Explore how it moulds nursing practice and is incorporated in reflective writing. Providing insights into practical application, this guide includes tips and strategies, underpinned by real examples. Moreover, you'll learn to navigate the challenges of reflective practice, honing a vital skill set for your nursing career.
Millions of flashcards designed to help you ace your studies
- Cell Biology
What are some tips for implementing Critical Reflection during clinical placements?
What is the role of reflective writing in nursing?
What is the relationship between critical reflection and clinical placements for nursing students?
What are some strategies for effective reflective writing in nursing?
What are some common mistakes in the process of critical reflection in nursing?
What is a suggested strategy for dealing with difficult situations during critical self-reflection in nursing?
What is the significance of reflective writing in nursing?
What is one way to overcome difficulties in applying the Gibbs Reflective Cycle in nursing?
What is the importance and role of Critical Reflection in nursing?
What is the concept of Critical Reflection in nursing?
What is the process of Critical Reflection in nursing?
Achieve better grades quicker with Premium
Geld-zurück-Garantie, wenn du durch die Prüfung fällst
Review generated flashcards
to start learning or create your own AI flashcards
Start learning or create your own AI flashcards

Vaia Editorial Team
Team Critical Reflection Teachers
- 16 minutes reading time
- Checked by Vaia Editorial Team
- Clinical Placement
- AACN Essentials
- Active Listening in Nursing
- Advanced Procedures
- Barriers in Communication in Nursing
- Basic Procedures
- Bedside Manners
- Blood Pressure Measurement
- Brazil Healthcare system
- Building Rapport
- CPR Training
- Canadian Medicare
- Catheterisation
- Clinical Assessment
- Clinical Competence
- Clinical Decision-Making
- Clinical Experience
- Clinical Exposure
- Clinical Judgment
- Clinical Learning Activities
- Clinical Learning Environment
- Clinical Learning Outcomes
- Clinical Outcomes
- Clinical Practice Guidelines
- Clinical Reasoning in Nursing
- Clinical Rotation
- Clinical Scenarios
- Clinical Simulation Scenarios
- Clinical Skill Demonstration
- Clinical Skills
- Clinical Skills Assessment
- Clinical Supervision
- Clinical Training
- Clustering Data
- Collaborative Interventions
- Collaborative Practice
- Comfort Care
- Communication Strategies in Healthcare
- Conflict Resolution
- Coordination of Care
- Critical Thinking in Nursing
- Cultural Responsiveness
- Direct Patient Care
- Disease Prevention
- E-learning modules
- Empathy in Nursing
- Error Reporting
- Ethical Principles in Nursing
- Ethical Standards
- France Healthcare System
- Germany Healthcare System
- Hands on Learning
- Health Assessment
- Health Care Delivery
- Health Care Policy
- Health Care Service
- Health Care System Structure
- Health Care Teamwork
- Health Promotion
- Health Teaching
- Healthcare Service Delivery
- Healthcare Systems
- Healthcare Team
- Hospital Protocol
- Human Error
- Hybrid Healthcare Systems
- IV Insertion
- Implicit Bias
- India Healthcare System
- Infection Control
- Interdisciplinary Collaboration
- Interpersonal Communications
- Japan Healthcare System
- Learning Opportunities
- Licensing Requirements
- Malpractice
- Medicare Australia
- Medication Administration
- Miscommunication in Nursing
- Morals in Nursing
- NHS Nursing
- Negligence in Nursing
- Non-therapeutic Communication
- Nurse Licensure Compact
- Nursing Care Assessment
- Nursing Care Delivery
- Nursing Care Plan Evaluation
- Nursing Care Plans
- Nursing Case Study
- Nursing Cues
- Nursing Diagnoses
- Nursing Documentation
- Nursing Education
- Nursing Inferences
- Nursing Interventions
- Nursing Judgment
- Nursing Outcomes Classification
- Nursing Procedures
- Nursing Process
- Patient Assessment
- Patient Care
- Patient Care Scenarios
- Patient Care Skills
- Patient Communication
- Patient Confidentiality
- Patient Education
- Patient Feedback
- Patient History Collection
- Patient Hygiene
- Patient Interaction
- Patient Interaction Skills
- Patient Management
- Patient Needs
- Patient Outcomes
- Patient Privacy
- Patient Safety
- Patient Safety Measures
- Patient-Centered Care
- Patient-Centered Interventions
- Private Healthcare
- Professional Accountability
- Professional Behavior
- Professional Ethics
- Professional Growth
- Professional Standards
- Public HealthCare
- Pulse and Respiratory Rate
- Recklessness
- SMART Goals
- Scope of Practice
- Simulation in Nursing Education
- Student Learning Objectives
- Swedish Healthcare System
- Teaching and Learning Methods in Nursing
- Team Communication
- Temperature Assessment
- Therapeutic Communication
- Therapeutic Interactions
- UK Healthcare System
- US Healthcare System
- US Medical Insurance
- Verbal Communication
- Virtual Reality Training
- Vital Signs
- Wellness Education
- Human Anatomy
- Intensive Care Nursing
- Mental Health Nursing
- Nursing Management
- Nursing Theories
- Types of Nursing
Jump to a key chapter
Understanding the Concept: What is Critical Reflection
In the world of nursing , there are several important concepts that you need to grasp in order to excel. Critical Reflection is one of these key concepts.
Critical Reflection is a crucial skill in the healthcare field. It involves systematically examining personal thoughts, feelings, and actions to learn from experiences and improve future practice. This deeper level of analysis can support both personal and professional development.
Importance and Role of Critical Reflection in Nursing
In the realm of nursing, Critical Reflection plays a fundamental role:
- It aids with problem-solving, encouraging you to reflect on possible outcomes before taking action.
- It supports lifelong learning, allowing you to identify areas of growth.
- It leads to improved patient care as reflecting on past actions can highlight areas for improvement.
By embracing Critical Reflection, nursing professionals can progressively cultivate a better understanding of both their strengths and the areas that need additional attention. It thus enables self-improvement throughout the professional journey.
Concept of Critical Self Reflection in Nursing
Within the sphere of Critical Reflection, there's an interesting sub-concept known as Critical Self Reflection.
Critical Self Reflection in nursing refers to the process of self-examination where nurses analyse their own thoughts, feelings, and actions. This introspective process contributes to personal growth and professional advancement, fostering higher levels of empathy and understanding toward patients.
A prime example of Critical Self Reflection is when a nurse dealing with a difficult patient stops to reflect on their handling of the situation. By asking questions like "Why did I react this way? Could I have better managed the situation? What can I learn from this for future interactions?", the nurse takes a critical look at their actions and emotions, leading to enhanced learning and better future practices.
The process of Critical Reflection
Understanding the process of Critical Reflection can give you a structure to follow. This process can be divided into a series of steps:
By going through these steps, you can assure that you thoroughly scrutinize your experiences, learn from them, and as a result, continually improve your practice.
Elaborating on the Critical Reflection Essay
A crucial aspect of practicing Critical Reflection in nursing is through the exercise of writing a Critical Reflection Essay. This is a type of academic writing where you, as a nursing professional, assess and scrutinize your experiences to gain insights and foster personal growth.
Structure and Components of a Critical Reflection Essay
A well-structured Critical Reflection Essay allows you to demonstrate your understanding of the material at hand, while simultaneously showcasing your ability to analyse your thoughts and experiences. Here are the key components of a Critical Reflection Essay:
Introduction
The introduction is where you delineate the subject of your reflection. This can be a specific event, patient interaction , or experience that sparked your reflection process. For instance, it could be based on a complex case that presented unique challenges.
The body of the essay is where greater depth of analysis is required. It is in this section you critically examine the event/experience, your responses to it, its impact on you, and the lessons learned. Emphasise on what you've learned about yourself as a nurse or about patient care in general.
The conclusion allows you to synthesise the results of your Critical Reflection. This is where you convey how your experience has impacted your professional growth and how it will inform future actions.
Incorporating Nursing Reflective Practice in your Essay
Reflective practice is central to nursing since it furthers learning and enriches patient care. Incorporating reflective practice in your essay requires you to deeply examine your thoughts, feelings, and actions to derive appropriate lessons.
Suppose you faced a challenging situation where a patient did not respond positively to a prescribed treatment. Instead of merely describing this event, you would, through reflection, delve into your thoughts and reactions during this incident. Additionally, you'll express how this experience has further informed your understanding of patient care and reactions.
Difference between Informal and Formal Reflective Writing
In the field of nursing, both formal and informal reflective writing are utilized, each having its unique features and purposes.
Informal Reflective Writing typically takes the form of diary entries or personal journal writing. It’s a more private, intimate form of reflection and has no strict format or structure. On the other hand, Formal Reflective Writing, such as a Critical Reflection Essay, is more structured and academic. Here, formal language is used, and the essay has a definitive structure comprising an introduction, body, and conclusion.
Importantly, both informal and formal reflective writing serve to foster a culture of learning and growth in nursing. Regardless of the form, effective reflective writing enables you, as a nursing professional, to engage in lifelong learning and continuous development.
Practical Aspects: Critical Reflection in Nursing
Moving beyond the theoretical understanding, let's now delve into the very practical aspect of Critical Reflection in nursing. In this section, you'll find a schema for reflective practice, practical examples, and tips on how to effectively implement Critical Reflection during clinical placement . These practical aspects are instrumental in guiding you towards becoming a reflective practitioner, thereby enhancing your nursing practice.
Making the Most out of the Gibbs Reflective Cycle in Nursing
Arguably one of the most accessible and widely-used models for structured reflection is the Gibbs Reflective Cycle. Having been developed by Graham Gibbs in 1988, this model encourages you to think systematically about the stages of an experience or activity. Here's the structure of the Gibbs Reflective Cycle:
Let's consider a practical example: You're a trainee nurse who's recently dealt with an aggressive patient. You might start by describing the event (Description), articulating how you felt during the interaction (Feelings) and evaluating both the positive and negative aspects (Evaluation). Following this, you'd analyse the event, concluding with what you learned and how you might handle such situations in the future (Analysis, Conclusion, Action Plan).
Practical Examples of Reflective Writing in Nursing
Understanding good reflective writing can be greatly aided by examining some practical examples. It's worth bearing in mind that while the content of reflective writing will be unique for everyone, certain structural features remain consistent. In particular, you need to focus on authenticity, introspection, and a clear line of development from description to analysis.
Suppose you're an emergency room nurse and you've experienced your first cardiorespiratory arrest in a patient. Your reflective write-up may express the initial shock and fear you faced (description and feelings), followed by an evaluation of your overall response. Your analysis could draw upon theoretical knowledge and consider if and how it supported your practical actions. Finally, your reflections might lead to a plan to identify additional training or support to handle similar situations in the future (action plan).
Tips for Implementing Critical Reflection During Clinical Placement
Understanding reflection and how to incorporate it into your practice will boost its effectiveness significantly. Here are a few pointers to help you embed Critical Reflection into your clinical placements:
- Start off by reflecting on concrete experiences, jotting down the thoughts, feelings, and lessons learned from these episodes.
- Embrace openness. The best reflections come from an honest appraisal of your actions and reactions, so refraining from self-judgement can be helpful.
- Regularly set aside time for reflection. This ensures that the process becomes a routine part of your professional practice.
- Consider using a reflective model like the Gibbs Reflective Cycle to structure your reflections.
- Always link theory with practice. This connectivity deepens the learning experience and encourages practical application of theoretical knowledge.
Bear in mind that reflection isn't solely about identifying areas for improvement. It's equally important to recognise what you did well—boosting confidence and reinforcing good practice. Balancing both of these aspects can lead to optimal personal and professional development.
The Art of Mastering your Nursing Reflective Practice
Having a grip on your nursing reflective practice is not just imperative, but it is also an art that requires quintessential skills. Reflective practice is essential for continual learning and improvement in your nursing career.
The Relationship Between Critical Reflection and Clinical Placement
The relationship between Critical Reflection and clinical placements is an intricate one. Clinical placements offer the perfect real-world settings for nursing students to apply what they have learned, and they are often the first contact students have with actual nursing practice.
Clinical placements offer nursing students a real-world scenario where nursing theory and practice become interlaced. During these placements, you will encounter a variety of patient cases, each offering their unique challenges and learning opportunities .
Here is where Critical Reflection becomes a handy tool. It allows you to pause, evaluate and learn from each experience, linking theory to practice, and inspiring continual improvement.
An instance of this is how during a clinical placement , you may encounter a challenging patient. Critical Reflection encourages you to analyse the situation beyond just figuring out the clinical solution. It propels you to delve deeper into your reaction, the decision-making process, the ethical considerations involved, the end result, and the lessons learned from the incident.
The Role of Reflective Writing in Nurturing Critical Thinking Skills
Reflective writing undoubtedly plays a significant role in fostering your critical thinking skills, better equipping you to deal with the challenges of nursing. It helps transform knowledge into know-how, bridging the gap between theoretical understanding and practical application.
Critical thinking, in the context of nursing, is the ability to reason, think logically, and make well-informed decisions, especially in high-pressure situations. It forms an essential part of clinical judgement and is fundamental to delivering quality patient care.
To illustrate, consider a situation where you are faced with a patient exhibiting symptoms of a stroke . Reflective writing can help you dissect your thought process like - How did you identify the symptoms? What treatment protocols followed, and why? How did you communicate with the patient and their family? How effective was the treatment, and what could you have done differently? By doing so, reflective writing nurtures your ability to think critically, enhancing decision-making and judgement in future instances.
Strategies for Effective Reflective Writing in Nursing
Reflective writing, when executed efficiently, can be an effective technique for improving your nursing skills. To achieve this, consider incorporating these strategies:
- Make it a Habit: Regularly dedicating time for reflective writing can help foster deeper insights and decode complex experiences.
- Think About Structure: Consider using a model for reflection, like Gibbs' or Kolb's, which provide a structured format to guide your thoughts.
- Be Honest: Reflective writing is for your benefit, so don't shy away from documenting your feelings, thoughts, or events exactly as they happened.
- Link Theory and Practice: By connecting what you study academically with what you experience during clinical practice, your understanding of nursing concepts will be reinforced.
- Follow an Iterative Process: Ensure to revise and update your reflections as your understanding evolves.
Always remember, the secret to effective reflective writing lies in authentic self-exploration and the readiness to learn and adapt. This practice of critical self-awareness not only betters your understanding of nursing concepts but also empowers you to become a more compassionate and effective healthcare provider .
Exploring the Challenges of Critical Reflection in Nursing
Though Critical Reflection is a crucial element of nursing practice, it does come with its own challenges. Unpacking these challenges aids in effective reflective practice, thereby enabling you to harness its true potential in clinical settings. Some common complications can include difficulties in setting aside personal biases, dealing with emotionally challenging situations, applying theoretical models to real-life events, and maintaining an objective perspective.
Common Mistakes in Critical Reflective Practice and How to Avoid Them
Familiarising yourself with common mistakes in reflective practice can serve as a guideline to steer clear of these pitfalls. Here are several inaccuracies that often crop up, along with tips on how to stay clear of them:
- Avoiding Emotionally Charged Events: Reflecting on emotional experiences is challenging, but it is in these instances that the most profound learning can occur. To sidestep this pitfall, view these occasions as opportunities for vital insight and professional growth .
- Overemphasis on Negative Aspects: Though critical analysis often involves identifying areas of improvement, calibrating it with the recognition of successful outcomes is equally important. This balanced approach ensures a more holistic reflection.
- Lack of Objectivity: While self-reflection is inherently personal, maintaining objectivity is crucial. To achieve this, consider describing the event as a neutral third party before analysing your emotions and reactions.
Imagine working on an emergency case where the patient, despite your best efforts, did not survive. Reflecting on such an incident could be emotionally draining. However, it can also provide insights into managing distressed families or making tough decisions under pressure. Additionally, instead of focusing only on what went wrong, acknowledging what went right can boost confidence and prepare you for similar future scenarios.
Overcoming Obstacles in Applying Gibbs Reflective Cycle in Nursing
Implementing a structured reflection model like the Gibbs Reflective Cycle has its hurdles. Here are some ways to navigate these roadblocks effectively:
- Difficulty in Recalling Feelings: It's natural to struggle with recalling emotions during an event, especially over time. To counteract this, try to pen down your reflections soon after an event when the experiences are fresh in your mind.
- Problem in Connecting Stages: The stages of the Gibbs cycle need to be connected and informed by one another. If you're having trouble with this, revisit each stage and draw out the links explicitly.
- Trouble in Formulating an Action Plan: Remember that action plans do not require drastic measures. Small changes or insights can be equally valuable. If you're stuck, consider discussing your thoughts with peers or mentors.
When used effectively, the Gibbs Reflective Cycle provides a framework that fosters a deeper understanding of your experiences, emotions, and thoughts, effectively bridging the gap between theory and practice. Always remember, proficiency comes with practice, so don't be dissuaded by early obstacles.
Tips for Dealing with Difficult Situations during Critical Self Reflection
Difficult situations, while challenging, can often become catalysts for profound learning and growth. Here are some strategies that can help navigate through these critical self-reflection moments:
- Keep a Non-judgemental Approach: Be honest in acknowledging your feelings, thoughts, and behaviours, without endorsing self-blame or criticism.
- Connect with Your Support System: Seek out those who provide emotional support and professional guidance when confronting difficult reflections.
- Maintain Confidentiality: While discussions can aid reflections, maintaining patient confidentiality is paramount.
- Practice Self-Care: Reflecting on emotionally taxing situations can be draining. Ensure to engage in activities that promote rest, relaxation, and wellness.
Consider a situation where a patient’s condition deteriorates rapidly despite your best efforts. Reflecting upon such situations can invoke feelings of inadequacy or guilt. However, by objectively analysing your actions, seeking guidance from your mentor, and taking out time to care for yourself, you can transform this experience into a pivotal learning opportunity.
Critical Reflection - Key takeaways
- Critical Reflection in nursing is the process of assessing and analyzing experiences to gain insights and foster personal growth.
- A Critical Reflection Essay is a specific type of academic writing used primarily in nursing, which includes an introduction, body, and conclusion.
- Informal Reflective Writing and Formal Reflective Writing are both used in nursing, with the former being more personal and format-less, and the latter being more structured and academic.
- The Gibbs Reflective Cycle is a model for structured reflection in nursing, which includes stages for description, feelings, evaluation, analysis, conclusion, and action plan.
- Critical Reflection during clinical placements allows students to evaluate and learn from their experiences, linking theory to actual nursing practice.
Flashcards in Critical Reflection 27
To implement Critical Reflection, start by reflecting on concrete experiences, be open and refrain from self-judgement. Regularly set aside time for reflection and consider using a reflective model like the Gibbs Reflective Cycle. Always link theory with practice for a richer learning experience.
Reflective writing fosters critical thinking skills, helping to transform knowledge into practical application. It aids in reasoning, logical thinking, and informed decision-making, particularly in high-pressure situations. It is key to clinical judgement and quality patient care.
Clinical placements offer a real-world scenario where theory and practice interlace. Critical reflection enables the evaluation and learning from each encounter, linking theory to practice, and encouraging continual improvement.
Strategies include making reflective writing a regular habit, using structured models for reflection like Gibbs' or Kolb's, being honest, linking theory and practice, and following an iterative process of revising and updating reflections.
Overemphasis on negative aspects, avoiding emotionally charged events and lack of objectivity are common mistakes in the critical reflection process in nursing.
A recommended strategy is to maintain a non-judgemental approach, being honest in acknowledging feelings, thoughts, and behaviours without endorsing self-blame or criticism.
Learn faster with the 27 flashcards about Critical Reflection
Sign up for free to gain access to all our flashcards.

Already have an account? Log in
Frequently Asked Questions about Critical Reflection
Test your knowledge with multiple choice flashcards, that was a fantastic start, you can do better, sign up to create your own flashcards.
Access over 700 million learning materials
Study more efficiently with flashcards
Get better grades with AI
Already have an account? Log in
Keep learning, you are doing great.
Discover learning materials with the free Vaia app

Vaia is a globally recognized educational technology company, offering a holistic learning platform designed for students of all ages and educational levels. Our platform provides learning support for a wide range of subjects, including STEM, Social Sciences, and Languages and also helps students to successfully master various tests and exams worldwide, such as GCSE, A Level, SAT, ACT, Abitur, and more. We offer an extensive library of learning materials, including interactive flashcards, comprehensive textbook solutions, and detailed explanations. The cutting-edge technology and tools we provide help students create their own learning materials. StudySmarter’s content is not only expert-verified but also regularly updated to ensure accuracy and relevance.
Team Nursing Teachers
Study anywhere. Anytime.Across all devices.
Create a free account to save this explanation..
Save explanations to your personalised space and access them anytime, anywhere!
By signing up, you agree to the Terms and Conditions and the Privacy Policy of Vaia.
Sign up to highlight and take notes. It’s 100% free.
Join over 22 million students in learning with our Vaia App
The first learning app that truly has everything you need to ace your exams in one place
- Flashcards & Quizzes
- AI Study Assistant
- Study Planner
- Smart Note-Taking

Privacy Overview
- LOGIN / FREE TRIAL

‘Let’s celebrate those who have a phenomenal impact on nursing’
STEVE FORD, EDITOR
- Assessment skills
- Children’s nursing
- Hospital nursing
- You are here: Opinion
‘Reflection is an often-misunderstood term within nursing’
13 April, 2022 By Nicola Clarke

Reflection is the exploration of experience, curiously investigating ourselves within the context of others and wider sphere of society and culture (Clarke, 2021).
Reflection uncovers the ‘why’ of our experiences. It generates knowledge about what constitutes ‘I’, raising self-awareness, leading to potential transformational change and generating knowledge to inform future experiences.
The process of reflection requires immersion within our experiences, being fully present with our thoughts and feelings, how we responded to others and our environment, and how we perceive how others respond to us. Reflection doesn’t require a critical incident to have an experience to learn from; it makes no assumption that we have done something wrong or need to improve. Reflection assumes a neutral position. We create a non-judgemental framework within which to empathically understand ourselves, in the context of professional practice and our many personal identities, which influence our behaviour in the clinical setting.
Reflection is required by the Nursing and Midwifery Council for revalidation every three years, using reflective discourse to learn from our experiences of continuing professional development, formalised in written accounts of learning. But we need to embody what it is to be the reflective practitioner outside the formal process, modelling this practice for our students in a profession that requires the therapeutic use of self.
The nursing profession requires us to create therapeutic relationships, sometimes called the therapeutic alliance. The most important factor in creating that alliance is you/us, who we are as people and how this infiltrates who we are as nurses. To deepen understanding of using the self therapeutically requires getting to know the self (Roberts, 2015). Taking that time out leads to an expression of self-care, not always realised in relationship to reflection. Exercise, sleeping seven hours and meditation are often considered self-care. We may not consider reflection as self-care, but essentially self-care is about allowing time out for us. Immersion within our experience, offering ourselves unconditional positive regard, being brave and honest enough to acknowledge our thoughts and feelings (Clarke, 2017) encourages productive time out within the reflective process.
“Reflection makes no assumption that we have done something wrong or need to improve”
How often do we allow ourselves to truly acknowledge and explore what we think and feel about our experiences? Narrating the movie of our lives, becoming our own filmmakers, first with a wide then a focused lens (Bolton and Delderfield, 2018), validates our narrative empathically; a notion often only applied to those we are caring for. Analysing our experience ensures purposeful thinking, not rumination, which potentially resolves internal conflict and remedies distortion of experience, leading to irrational guilt.
Drawing upon the wider sphere (such as literature, feedback and observation) allows us to view our experiences from different perspectives, enabling objectivity into the subjective. Drawing conclusions about the meaning of experience facilitates personal growth and understanding that may lead to insights to inform our future experiences (Greenberger, 2020), empowering us to be the best version of ourselves.
Recommended
Reflective practice 1: aims, principles and role in revalidation
Visit NT's Opinion section
Popularity of the notion of reflection means its meaning is often assumed to be obvious, and its teaching within higher education has historically been overlooked or introduced formally in a momentary manner (Roberts, 2015). Reflection is also an often-misunderstood term. Evaluation and incident analysis can be misrepresented as reflection, reducing it to what did and didn’t go well to create actions to improve practice, reducing student engagement with the reflective process.
Introducing reflection to students as just bound by reflective models and frameworks risks reflection being viewed as a recipe or instructions for making something (Bolton and Delderfield, 2018). Learning is a dynamic process and reflection should be taught as an organic activity that can be messy and occur as a solo activity, in written format or as part of a facilitated reflective conversation.
As nursing academics and practice assessors/supervisors, we need to upskill, so we not only engage in the reflective process and model reflective behaviour correctly, but also offer students guided discovery, embedded in the nursing curriculum and the clinical area.
Nicola Clarke is senior lecturer at the Faculty of Health Education and Life Sciences, Birmingham City University
Bolton G, Delderfield R (2018) Reflective Practice; Writing and Professional Development . SAGE Publications Ltd.
Clarke NM (2021) Experience, Deconstruction, Implementation: EDI; A new approach to reflective writing for academic purpose. Reflective Practice ; 22: 5, 714-726.
Clarke NM (2017) The Student Nurses Guide to Successful Reflection: Ten Essential Ingredients. McGraw Hill Education.
Greenberger SW (2020) Creating a guide for reflective practice: applying Dewey’s reflective thinking to document faculty scholarly engagement. Reflective Practice ; 21: 4, 458–472
Roberts M (2015) Critical Thinking and Reflection for Mental Health Nursing Students . SAGE Publications Ltd.
- Add to Bookmarks
One comment
I found the articles I have read thought provoking. I have viewed reflection as a negative experience something I have done wrong. I always try to learn from it but I can ruminate and catastrophes which is not constructive. We are all bound by time constraints and there is no ideal situation.it takes time to assess a patient and even with prior knowledge and a good background history we do not always have the tools we need to make a rapid evaluation.hindsight is a wonderful thing but does it just give us time to focus on all the things we did wrong and not on the things that we got right and we can improve on in the future lm going to try to take this forward with me.
Have your say
Sign in or Register a new account to join the discussion.

IMAGES
COMMENTS
The process of critical self-reflection can foster transformational learning in adults, which Mezirow (1990) attributes to reflection’s higher-order mental process. This leads to: 1) rational examination of assumptions, 2) action based on the question What am I doing wrong?, 3) focus on presuppositions that relate to a problem, and 4 ...
develop reflective practice and that this can be used as evidence in their assessments. 1.2 prioritise the wellbeing of people promoting critical self-reflection and safe practice in accordance with the Code 1.8 ensure mistakes and incidents are fully investigated and learning reflections and actions are recorded and disseminated
Reflective Practice in Nursing: A Guide to Improving Patient Care -Reflective practice is an important aspect of nursing that involves the critical analysis of one’s own experiences and actions to improve nursing practice. It is a process of self-reflection and self-evaluation that can lead to personal and professional growth. This article ...
Mar 16, 2023 · The critical thinking of clinical nurses is essential for identifying the needs of patients and providing safe care through prompt and accurate judgment [1,2,3].Critical thinking can be practiced through critical reflection [], a dynamic process in which nurses reflect on their nursing behavior to improve their perspective on a situation and change future nursing practices in a desirable ...
Self-reflection becomes critical when it goes beyond mere reflection, questioning teaching assumptions, and addressing their social and political context. Given the remarked benefits of using self-reflection in education, and the current COVID-19 global repercussions which have urged faculties to try alternative methods of teaching, a concise ...
Jul 30, 2024 · The connection between self-reflection, self-efficacy, and work engagement. Using a stratified random sampling method and inclusion criteria that included holding a bachelor’s degree in nursing and clinical working experience, a total of 240 nurses from seven hospitals were selected for the study. 3 Data were collected via three questionnaires: Groningen Reflection Ability Scale (GRAS ...
Jan 1, 2021 · Legare and Armstrong (2017) refer to critical self-reflection as a deeper state of personal reflection, one which was found to support the transition from clinical practice to the nursing faculty, however, a more appropriate definition that looks beyond deep reflection to ensure comprehensiveness, was provided by Brookfield (2017).
The critical reflection competency program was effective in improving the critical thinking disposition and teaching efficacy of nurse educators. Therefore, it is necessary to implement the developed program for nurse educators to effectively utilize critical reflection in nursing education.
Critical Self Reflection in nursing refers to the process of self-examination where nurses analyse their own thoughts, feelings, and actions. This introspective process contributes to personal growth and professional advancement, fostering higher levels of empathy and understanding toward patients.
Apr 13, 2022 · We may not consider reflection as self-care, but essentially self-care is about allowing time out for us. Immersion within our experience, offering ourselves unconditional positive regard, being brave and honest enough to acknowledge our thoughts and feelings (Clarke, 2017) encourages productive time out within the reflective process.