An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Child Trauma Exposure and Psychopathology: Mechanisms of Risk and Resilience
Katie a mclaughlin , ph.d., hilary k lambert.
- Author information
- Copyright and License information
The corresponding author is Katie A. McLaughlin. Contact information is as follows: Katie A. McLaughlin, Ph.D., Department of Psychology, University of Washington, Box 351525, Seattle, WA 98195, 206-616-7863, [email protected]
Hilary K. Lambert, Department of Psychology, University of Washington, Box 351525, Seattle, WA 98195, 206-221-8030, [email protected]
Exposure to trauma in childhood is associated with elevated risk for multiple forms of psychopathology. Here we present a biopsychosocial model outlining the mechanisms that link child trauma with psychopathology and protective factors that can mitigate these risk pathways. We focus on four mechanisms of enhanced threat processing: information processing biases that facilitate rapid identification of environmental threats, disruptions in learning mechanisms underlying the acquisition of fear, heightened emotional responses to potential threats, and difficulty disengaging from negative emotional content. Supportive relationships with caregivers, heightened sensitivity to rewarding and positive stimuli, and mature amygdala-prefrontal circuitry each serve as potential buffers of these risk pathways, highlighting novel directions for interventions aimed at preventing the onset of psychopathology following child trauma.
Exposure to trauma in childhood is a risk factor for many forms of psychopathology, including post-traumatic stress disorder (PTSD), anxiety, depression, disruptive behaviors, and substance abuse [ 1 – 4 ]. Risk for psychopathology following trauma is most pronounced in children exposed to interpersonal violence [ 1 , 3 , 4 ]. Identifying mechanisms that underlie the strong link between child trauma and psychopathology as well as factors that buffer this risk is critical in order to develop targets for preventive interventions. In this paper, we review mechanisms that underlie vulnerability to psychopathology following child trauma and protective factors that mitigate risk pathways (see Figure 1 ). Specifically, we highlight the role of disruptions in threat processing as a central mechanism linking child trauma to multiple forms of psychopathology and identify protective factors spanning social, emotional, and neurobiological levels that may buffer children from the negative mental health consequences of trauma exposure. We specifically focus on innovative recent discoveries and factors that could be directly targeted with psychosocial interventions.
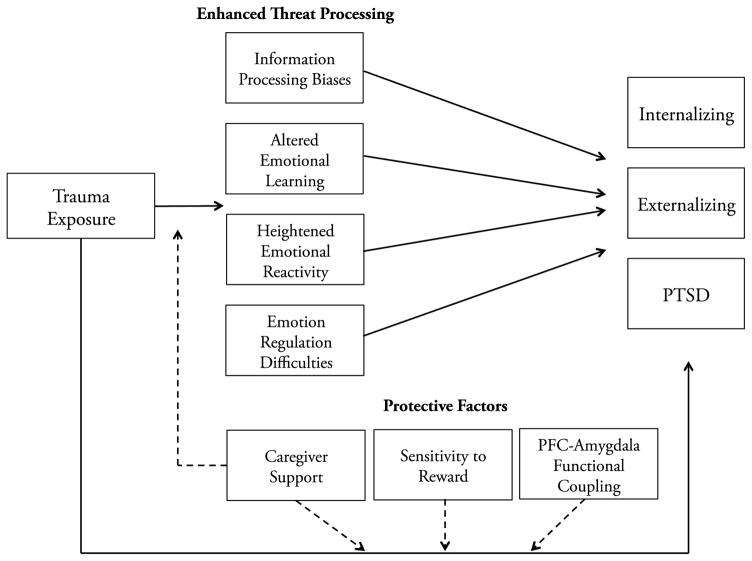
A biopsychosocial model of risk and resilience to psychopathology following child trauma.
This figure depicts a biopsychosocial model of mechanisms linking child trauma with psychopathology and protective factors that mitigate risk pathways. Solid lines reflect direct associations between child trauma and threat processing and between threat processing and psychopathology. Enhanced threat processing is a transdiagnostic factor associated with multiple forms of child psychopathology. Each domain of threat processing is associated with internalizing and externalizing psychopathology, as well as post-traumatic stress disorder (PTSD); although greater research is needed to clarify whether the specific disruptions in emotional learning associated with child trauma are associated with mental health problems other than externalizing psychopathology. PTSD is depicted separately from internalizing and externalizing problems given its current classification as a trauma and stressor-related disorder in DSM-5. Dashed lines represent the buffering effect of each of the protective factors on specific risk pathways.
Trauma Exposure and Threat Processing
Traumatic events involve harm or threat of harm [ 5 ]. This is particularly true for traumatic events involving exposure to interpersonal violence, including physical abuse, sexual abuse, witnessing domestic violence, and exposure to other forms of violence in the home or community. Approximately one in five children in the U.S. will experience a traumatic event involving interpersonal violence by the time they reach adulthood [ 4 ]. Exposure to these types of traumatic events in childhood alters affective and neurobiological development to enhance the identification of potential threats in the environmental and magnify emotional responses to those threats. Although these adaptations may promote safety in dangerous environments, they are a central mechanism linking child trauma to the onset of both internalizing and externalizing psychopathology. We review evidence for heightened threat processing at multiple levels—including social information processing biases, altered emotional learning, elevated emotional reactivity, and emotion regulation difficulties—as a developmental mechanism linking child trauma with psychopathology. Given that disruptions in threat processing and risk for psychopathology are particularly pronounced in children who have experienced interpersonal violence, we focus primarily on this form of child trauma exposure. We constrain our review to domains of threat processing that present plausible targets for psychosocial interventions, although additional mechanisms clearly play a role in the pathways linking child trauma to psychopathology, including changes in stress hormones and epigenetic factors [ 6 ].
Social Information Processing Biases
Trauma-exposed children exhibit information processing biases that facilitate rapid identification of environmental threats. One such bias involves heightened perceptual sensitivity to anger. Children with trauma histories identify anger with less perceptual information and classify a wider range of emotions as anger than children who have never experienced trauma [ 7 – 9 ]. Trauma-exposed children also exhibit attention biases to threatening social information [ 10 ], including faster attentional engagement and delayed attentional disengagement from anger [ 11 , 12 ]. In social situations, extensive evidence documents that children exposed to trauma are more likely to attend to threatening cues, ignore non-threatening cues, and generate hostile attributions than children without trauma histories [ 13 ].
Enhanced threat processing may occur at the expense of processing non-emotional aspects of the environment. Specifically, trauma-exposed children have poor memory for contextual information that occurs in the background of threatening cues as well as reduced activation of the hippocampus and atypical hippocampal-prefrontal cortex functional connectivity when contextual encoding occurs in the presence of threat [ 14 ]. Heightened attention to threat following child trauma may interfere with processing contextual information that could help children discriminate between safe and dangerous environments. This pattern might ultimately contribute to psychopathology by making it difficult for children to contextualize cues that have previously been associated with threat, leading to persistent fear even in safe environments.
These disruptions in social information processing are developmental mechanisms that underlie the association of child trauma with anxiety [ 12 ], PTSD [ 15 ], aggression and conduct problems [ 10 , 13 ].
Altered Emotional Learning
Disruptions in learning processes involved in the acquisition and extinction of conditioned fear are considered a central mechanism in the etiology of trauma-related psychopathology [ 16 ], but have rarely been studied in children. A recent study shows that whereas children without trauma exposure exhibit robust discrimination in skin conductance responses (SCR) during fear conditioning between cues that predict threat (CS+) and safety (CS−), trauma-exposed children fail to discriminate between threat and safety cues, exhibiting SCR of similar magnitude to both types of cues [ 17 ]. This pattern could reflect either generalization of fear, whereby children exposed to trauma interpret a wider range of cues as potential threats, or difficulty learning safety signals. Poor threat-safety discrimination mediates the association of child trauma with externalizing problems [ 17 ], indicating that perturbed fear learning is a potential mechanism linking child trauma to psychopathology.
Heightened Emotional Reactivity
Children exposed to trauma exhibit exaggerated emotional responses to negative stimuli that could signal the presence of threat, which serves as an additional mechanism linking child trauma with psychopathology. Heightened emotional reactivity following child trauma has been observed at both state and trait levels [ 18 , 19 ], and in magnified negative emotional reactions to daily stressors in adulthood [ 20 ]. Elevated amygdala response to numerous types of negative stimuli has been observed among trauma-exposed children [ 21 – 23 ], suggesting that negative emotional cues are particularly salient following child trauma. Atypical physiological responses to stress have been consistently observed in trauma-exposed children. Here we focus on recent work examining physiological patterns based on a well-validated model of threat responding, where threat appraisals produce a pattern of autonomic nervous system (ANS) response characterized by increased sympathetic nervous system activation but constricted cardiac output (i.e., blood flow from the heart) due to peripheral vasoconstriction [ 24 ]. Two studies have documented this threat pattern of ANS reactivity to stress among adolescents with trauma histories [ 25 , 26 ].
Magnified emotional reactivity to negative stimuli is associated with concurrent psychopathology [ 25 , 26 ] and mediates the association of child trauma with both internalizing and externalizing problems [ 18 , 27 , 28 ]. Heightened amygdala response to negative stimuli assessed prior to trauma exposure predicts the onset of PTSD symptoms following a traumatic stressor [ 29 ] and increases in internalizing symptoms following stressful life events [ 30 ].
Emotion Regulation Difficulties
Trauma-exposed children also experience disruptions in emotion regulation that make it difficult to disengage from negative emotional content. For example, frequent engagement in rumination—a strategy characterized by repetitive thought about the causes and consequences of distress—is common among trauma-exposed children [ 18 ]. Effortful emotion regulation strategies that modulate responses to negative stimuli, such as cognitive reappraisal, require greater cognitive resources or effort for children who have experienced trauma; when engaging in cognitive reappraisal, children exposed to trauma recruit prefrontal cortex regions involved in cognitive control to a great degree than children without trauma exposure [ 23 ]. Several recent studies have documented poor adaptation to emotional conflict, a form of implicit emotion regulation, among trauma-exposed children [ 31 , 32 ]. These trauma-related behavioral differences are mediated by reduced functional coupling of amygdala and medial prefrontal cortex (mPFC) [ 32 ]. The mPFC inhibits the amygdala in numerous forms of implicit emotion regulation. Reduced resting-state mPFC-amygdala functional connectivity has been observed in multiple studies of trauma-exposed adolescents [ 33 , 34 ], highlighting a potential neural substrate of implicit emotion regulation difficulties.
Patterns of emotion regulation observed in trauma-exposed children have been associated consistently with youth internalizing and externalizing psychopathology [ 35 , 36 ], and, when measured prior to trauma exposure, predict the subsequent onset of PTSD symptoms following a traumatic event [ 37 ]. Longitudinal studies confirm that emotion regulation difficulties are a mechanism linking child trauma to the onset of internalizing and externalizing symptoms [ 18 , 38 ].
Protective Factors
Protective factors spanning social, emotional, and neurobiological domains may buffer children either from enhanced threat processing or from experiencing psychopathology following exposure to trauma.
Caregiver Support
Relationships with caregivers play a key role in protecting children from the onset of trauma-related psychopathology. Meta-analytic evidence indicates that children who have supportive caregivers are less likely to develop psychopathology following trauma exposure [ 39 ]. Recent work highlights a potential mechanism for this protective effect: maternal buffering of threat processing. Cues that signal maternal presence are associated with dampened amygdala reactivity and greater mPFC-amygdala functional connectivity in children, particularly those who have a supportive relationship with their mother [ 40 ]. Similarly, maternal presence enhances threat-safety discrimination during fear conditioning in children [ 41 ]. Critically, amygdala reactivity to threatening cues following trauma exposure is weaker in children with high maternal support [ 42 ]. Together, these findings suggest that one pathway through which social support might confer protection from trauma-related psychopathology is by dampening threat processing after a traumatic event.
Sensitivity to Reward
Sensitivity to positive and rewarding stimuli at both neural and behavioral levels is associated with reduced risk for psychopathology following child trauma exposure. Child trauma is associated with anhedonia less strongly in young adults with high ventral striatum reactivity to reward [ 43 ]. Lower levels of anhedonia, in turn, are associated with reduced depression symptoms and problematic drinking following child trauma [ 43 ]. Similarly, child trauma is not associated with depression, either concurrently or prospectively, among adolescents who exhibit high behavioral sensitivity to reward during a reward-processing task or who exhibit high reactivity to positive social stimuli in the pallidum and putamen—basal ganglia regions implicated in reward processing [ 44 ]. These findings are consistent with evidence that the association of stressful life events with depression is weaker among individuals with high ventral striatum reactivity to reward [ 45 ]. Accumulating evidence suggests that sensitivity to rewarding and positive cues may protect against the development of trauma-related psychopathology. Identifying the mechanism of this protective effect is an important direction for future research.

Mature Prefrontal-Amygdala Circuitry
As reviewed above, child trauma influences numerous forms of emotion regulation and the neural circuitry that supports effective regulation. However, some aspects of emotion regulation ability appear to interact with childhood adversity, serving as a protective factor against the development of internalizing psychopathology. Two recent studies suggest that greater mPFC-amygdala functional coupling—a marker of mature emotion regulation neural circuitry [ 46 ]—is a protective factor that buffers children from the onset of psychopathology following environmental adversity. In both studies, greater mPFC-amygdala functional connectivity during a threat-processing task predicts lower levels of internalizing psychopathology among children who experienced early adversity—including institutional rearing and diverse family-related stressors [ 47 , 48 ]. Greater research is needed to clarify the direct links between trauma and mPFC-amygdala circuitry and the circumstances in which this circuitry protects against trauma-related psychopathology.
Intervention Implications
Numerous evidence-based interventions exist for treating trauma-related psychopathology in youth [ 49 ]. Cognitive behavioral therapy (CBT) is currently the most well-established treatment for child trauma-related psychopathology [ 49 ] and targets many of the threat processing mechanisms reviewed here. CBT for child trauma targets social information processing biases with cognitive coping techniques, emotional learning with imaginal and in vivo exposure, emotional reactivity with relaxation training, and emotion regulation with affective modulation skills. CBT also incorporates parents into the treatment with techniques aimed at improving parenting skills and bolstering the parent-child relationship. These components may further improve caregiver support, a key protective factor that buffers children from trauma-related psychopathology. A critical future direction for the field is to determine whether these intervention techniques targeting threat processing and caregiver support can prevent the onset of psychopathology in children exposed to trauma. One study shows promising results of a skill-based intervention delivered to both parents and children in preventing child PTSD and anxiety 3-months following trauma exposure [ 50 ]. It is currently unknown whether interventions targeting reward processing (e.g., behavioral activation) can prevent trauma-related psychopathology, as these approaches have yet to be examined empirically in children with trauma exposure. Greater research on preventive interventions following child trauma is clearly needed.
Disruptions in threat processing are a key neurodevelopmental mechanism underlying the associations between child trauma and the onset of psychopathology. Enhanced threat processing occurs at multiple levels, including information processing biases, altered emotional learning, enhanced emotional reactivity, and poor emotion regulation. Supportive relationships with caregivers, heightened sensitivity to rewarding and positive stimuli, and mature prefrontal-amygdala circuitry each serve as potential buffers of these risk pathways, highlighting novel directions for interventions aimed at preventing the onset of psychopathology following child trauma.
Highlights.
Enhanced threat processing is a mechanism linking child trauma to psychopathology
Information processing biases and altered emotional learning are key mechanisms
Heightened emotional reactivity and poor emotion regulation are additional pathways
Supportive relationships with caregivers may reduce threat processing
Sensitivity to reward and mature amygdala-prefrontal circuitry are also protective
Acknowledgments
This research was supported by grants from the National Institutes of Health (R01-MH103291 and R01-MH106482), the Brain and Behavior Foundation (Young Investigator Award), the Jacobs Foundation (Early Career Research Fellowship), and a Rising Star Research Award grant from AIM for Mental Health, a program of One Mind Institute (IMHRO) to McLaughlin.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References and Recommended Reading
Papers of particular interest, published within the period of review, have been highlighted as:
* of special interest
**of outstanding interest
- 1. McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky A, Kessler RC. Childhood adversities and first onset of psychiatric disorders in a national sample of adolescents. Archives of General Psychiatry. 2012;69:1151–1160. doi: 10.1001/archgenpsychiatry.2011.2277. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Carliner H, Keyes KM, McLaughlin KA, Meyers JL, Dunn EC, Martins SS. Childhood trauma and illict drug use in adolescence: A population-based National Comorbidity Survey Replication-Adolescent Supplement study. Journal of the American Academy of Child & Adolescent Psychiatry. 2016;55:701–708. doi: 10.1016/j.jaac.2016.05.010. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Alisic E, Zalta AK, van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, Smid GE. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. British Journal of Psychiatry. 2014;204:335–340. doi: 10.1192/bjp.bp.113.131227. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. McLaughlin KA, Koenen KC, Hill E, Petukhova M, Sampson NA, Zaslavsky A, Kessler RC. Trauma exposure and posttraumatic stress disorder in a US national sample of adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:815–830. doi: 10.1016/j.jaac.2013.05.011. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. McLaughlin KA, Sheridan MA, Lambert HK. Childhood Adversity and Neural Development: Deprivation and Threat as Distinct Dimensions of Early Experience. Neuroscience and Biobehavioral Reviews. 2014;47:578–591. doi: 10.1016/j.neubiorev.2014.10.012. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. McCrory E, De Brito SA, Viding E. The impact of childhood maltreatment: a review of neurobiological and genetic factors. Frontiers in Psychiatry. 2011:2. doi: 10.3389/fpsyt.2011.00048. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Pollak SD, Sinha P. Effects of early experience on children’s recognition of facial displays of emotion. Development and Psychopathology. 2002;38:784–791. doi: 10.1037//0012-1649.38.5.784. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Pollak SD, Cicchetti D, Hornung K, Reed A. Recognizing emotion in faces: Developmental effects of child abuse and neglect. Developmental Psychology. 2000;36:679–688. doi: 10.1037/0012-1649.36.5.679. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Pollak SD, Kistler DJ. Early experience is associated with the development of categorical representations for facial expressions of emotion. Proceedings of the National Academy of Sciences. 2002;99:9072–9076. doi: 10.1073/pnas.142165999. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Shackman JE, Pollak SD. Impact of physical maltreatment on the regulation of negative affect and aggression. Development and Psychopathology. 2014;26:1021–1033. doi: 10.1017/S0954579414000546. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Pollak SD, Tolley-Schell SA. Selective attention to facial emotion in physically abused children. Journal of abnormal psychology. 2003;112:323–338. doi: 10.1037/0021-843x.112.3.323. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Shackman JE, Shackman AJ, Pollak SD. Physical abuse amplifies attention to threat and increases anxiety in children. Emotion. 2007;7:838–842. doi: 10.1037/1528-3542.7.4.838. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Dodge KA, Petit GS, Bates JE, Valente E. Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. Journal of Abnormal Psychology. 1995;104:632–643. doi: 10.1037//0021-843x.104.4.632. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Lambert HK, Sambrook K, Sheridan MA, Rosen ML, Askren MK, McLaughlin KA. The role of the hippocampus in context encoding and disruption following violence exposure in youth. Journal of Neuroscience. 2016 [ Google Scholar ]
- 15. Briggs-Gowan MJ, Grasso D, Bar-Haim Y, Voss J, McCarthy KJ, Pine DS, Wakschlag LS. Attention bias in the developmental unfolding of posttraumatic stress symptoms in young children at risk. Journal of Child Psychology and Psychiatry. doi: 10.1111/jcpp.12577. in press. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Lissek S, van Meurs B. Learning models of PTSD: Theoretical accounts and psychobiological evidence. International Journal of Psychophysiology. 2015;98:594–605. doi: 10.1016/j.ijpsycho.2014.11.006. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17*. McLaughlin KA, Sheridan MA, Gold AL, Lambert HK, Heleniak C, Duys A, Shechner T, Wojcieski Z, Pine DS. Maltreatment exposure, brain structure, and fear conditioning in children. Neuropsychopharmacology. 2016;41:1956–1964. doi: 10.1038/npp.2015.365. Children who had never experienced maltreatment exhibited strong differential conditioning to threat and safety cues based on skin conductance responses (SCR) and self-reported fear in a fear conditioning task. In contrast, maltreated children exhibited reduced SCR to the threat cue and failed to show a differential SCR to the threat and safety cues during early fear conditioning. Poor threat-safety discrimination mediated the association of child maltreatment with externalizing psychopathology. Disruptions in fear learning processes may underlie the development of psychopathology following child maltreatment. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Heleniak C, Jenness J, Van der Stoep A, McCauley E, McLaughlin KA. Childhood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research. 2016;40:394–415. doi: 10.1007/s10608-015-9735-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Hennessy KD, Rabideau GJ, Cicchetti D, Cummings EM. Responses of physically abused and nonabused children to different forms of interadult anger. Child Development. 1994;65:815–828. [ PubMed ] [ Google Scholar ]
- 20. Wichers M, Schrijvers D, Geschwind N, Jacobs N, Myin-Germeys I, Thiery E, Derom C, Sabbe B, Peeters F, Delespaul P, et al. Mechanisms of gene-environment interactions in depression: evidence that genes potentiate multiple sources of adversity. Psychological Medicine. 2009;39:1077–1086. doi: 10.1017/S0033291708004388. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. McCrory EJ, De Brito SA, Sebastian CL, Mechelli A, Bird G, Kelly PA, Viding E. Heightened neural reactivity to threat in child victims of family violence. Current Biology. 2011;21:R947–948. doi: 10.1016/j.cub.2011.10.015. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Suzuki H, Luby JL, Botteron KN, Dietrich R, McAvoy MP, Barch DM. Early life stress and trauma and enhanced limbic activation to emotionally valenced faces in depressed and healthy children. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53:800–813. doi: 10.1016/j.jaac.2014.04.013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23*. McLaughlin KA, Peverill M, Gold AL, Alves S, Sheridan MA. Child maltreatment and neural systems underlying emotion regulation. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54:753–762. doi: 10.1016/j.jaac.2015.06.010. Children exposed to maltreatment exhibited heightened amygdala response to negative, but not positive, stimuli. When engaging in cognitive reappraisal to modulate responses to negative stimuli, maltreated children recruited regions in the dorsal-lateral and medial prefrontal cortex to a greater degree than non-maltreated youths but modulated the amygdala to a similar degree. Child maltreatment heightens the salience of negative emotional stimuli; as a result, maltreated children may require greater cognitive resources than non-maltreated children to modulate their responses to negative stimuli. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 24. Mendes WB, Major B, McCoy S, Blascovich J. How attributional ambiguity shapes physiological and emotional responses to social rejction and acceptance. Journal of Personality and Social Psychology. 2008;94:278–291. doi: 10.1037/0022-3514.94.2.278. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. McLaughlin KA, Sheridan MA, Alves S, Mendes WB. Child maltreatment and autonomic nervous system reactivity: Identifying dysregulated stress reactivity patterns using the biopsychosocial model of challenge and threat. Psychosomatic Medicine. 2014;76:538–546. doi: 10.1097/PSY.0000000000000098. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Heleniak C, McLaughlin KA, Ormel J, Riese H. Autonomic nervous system reactivity as a mechanism linking child trauma to adolescent psychopathology. Biological Psychology. doi: 10.1016/j.biopsycho.2016.08.007. in press. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Kim-Spoon J, Cicchetti D, Rogosch FA. A longitudinal study of emotion regulation, emotion lability-negativity, and internalizing symptomatology in maltreated and nonmaltreated children. Child Development. 2013;84:512–527. doi: 10.1111/j.1467-8624.2012.01857.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. McLaughlin KA, Kubzansky LD, Dunn EC, Waldinger RJ, Vaillant GE, Koenen KC. Childhood social environment, emotional reactivity to stress, and mood and anxiety disorders across the life course. Depression and Anxiety. 2010;27:1087–1094. doi: 10.1002/da.20762. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29**. McLaughlin KA, Busso DS, Duys A, Green JG, Alves S, Way M, Sheridan MA. Amygdala response to negative stimuli predicts PTSD symptom onset following a terrorist attack. Depression and Anxiety. 2014;10:834–842. doi: 10.1002/da.22284. Heightened amygdala response to negative emotional cues assessed prior to exposure to a terrorist attack was associated with the subsequent onset of post-traumatic stress disorder (PTSD) symptoms in adolescents following the attack. Elevations in amygdala reactivity to negative cues, commonly observed among children exposed to trauma, may confer risk for the onset of PTSD following exposure to traumatic events. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Swartz JR, Knodt AR, Radtke SR, Hariri AR. A neural biomarker of psychological vulnerability to future life stress. Neuron. 2015;85:505–511. doi: 10.1016/j.neuron.2014.12.055. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Lambert HK, King KM, Monahan KC, McLaughlin KA. Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Development and Psychopathology. doi: 10.1017/S0954579416000584. in press. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Marusak HA, Martin KR, Etkin A, Thomason ME. Childhood trauma exposure disrupts the automatic regulation of emotional processing. Neuropsychopharmacology. 2015;40:1250–1258. doi: 10.1038/npp.2014.311. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 33. Herringa RJ, Birn RM, Ruttle PL, Stodola DE, Davidson RJ, Essex MJ. Childhood maltreatment is associated with altered fear circuitry and increased internalizing symptoms by late adolescence. Proceedings of the National Academy of Sciences. 2013;110:19119–19124. doi: 10.1073/pnas.1310766110. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 34. Thomason ME, Marusak HA, Tocco MA, Vila AM, McGarragle O, Rosenberg DR. Altered amygdala connectivity in urban youth exposed to trauma. Social Cognitive and Affective Neuroscience. 2015 doi: 10.1093/scan/nsv030. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. McLaughlin KA, Hatzenbuehler ML, Mennin DS, Nolen-Hoeksema S. Emotion regulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy. 2011;49:544–554. doi: 10.1016/j.brat.2011.06.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Michl LC, McLaughlin KA, Shepherd K, Nolen-Hoeksema S. Rumination as a mechanism linking stressful life events to symptoms of depression and anxiety: Longitudinal evidence in early adolescents and adults. Journal of Abnormal Psychology. 2013;122:339–352. doi: 10.1037/a0031994. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Jenness J, Jager-Hyman S, Heleniak C, Beck AT, Sheridan MA, McLaughlin KA. Catastrophizing, rumination, and reappraisal prospectively predict adolescent PTSD symptom onset following a terrorist attack. Depression and Anxiety. doi: 10.1002/da.22548. in press. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry. 2010;51:706–716. doi: 10.1111/j.1469-7610.2009.02202.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 39. Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32:122–138. doi: 10.1016/j.cpr.2011.12.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40*. Gee DG, Gabard-Durnam LJ, Telzer EH, Humphreys KL, Goff B, Shapiro M, Flannery J, Lumian DS, Fareri DS, Caldera C, et al. Maternal buffering of human amygdala-prefrontal circuitry during childhood but not during adolescence. Psychological Science. 2014;25:2067–2078. doi: 10.1177/0956797614550878. Children exhibited enhanced negative functional connectivity between the medial prefrontal cortex and amygdala, reduced amygdala reactivity, and enhanced affect regulation in response to maternal facial expressions than to stranger facial expressions. This pattern was not observed among adolescents, who exhibited mature patterns of medial prefrontal cortex-amygdala negative coupling, amygdala reactivity, and affect regulation in response to all facial expressions. Caregivers promote emotion regulation in children with immature emotion regulation circuitry. Adolescents have mature emotion regulation circuitry and therefore do not rely on external sources to regulate their emotions. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. van Rooij SJH, Cross D, Stevens JS, Vance LA, Kim YJ, Bradley BP, Tottenham N, Jovanovic T. Maternal buffering of fear-potentiated startle in children and adolescents with trauma exposure. Social Neuroscience. doi: 10.1080/17470919.2016.1164244. in press. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Orr C, Hudziak JJ, Albaugh M, Carlozzi B, Holbrook H, O’Loughlin K, Garavan H, Kaufman J. Society of Biological Psychiatry, editor. Social supports moderate the effects of child maltreatment on neural correlates of threat processing. Atlanta, GA: 2016. [ Google Scholar ]
- 43. Corral-Frias NS, Nikolova YS, Michalski LJ, Baranger DAA, Hariri AR, Bogdan R. Stress-related anhedonia is associated with ventral striatum reactivity to reward and transdiagnostic psychiatric symptomatology. Psychological Medicine. 2015;45:2605–2617. doi: 10.1017/S0033291715000525. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 44**. Dennison MJ, Sheridan MA, Busso DS, Jenness JL, Peverill M, Rosen ML, McLaughlin KA. Neurobehavioral markers of resilience to depression amongst adolescent exposed to child abuse. Journal of Abnormal Psychology. in press Adolescents exposed to child maltreatment exhibited no elevations in depression symptoms compared to non-maltreated youths when they had high sensitivity to reward across neural and behavioral measures. High sensitivity to reward was reflected in greater activity in the left pallidum to positive social images and faster reaction time to cues paired with monetary reward relative to those unpaired with reward in a reward-processing task. Greater activity in the left putamen in response to positive images moderated the association of maltreatment with depression over time, such that maltreatment was not associated with increases in depression over time among youths with high putamen response to positive cues. Reactivity to rewarding and positive cues, at both neural and behavioral levels, is a potential marker of resilience to depression among adolescents exposed to maltreatment. [ Google Scholar ]
- 45. Nikolova YS, Bogdan R, Brigidi BD, Hariri AR. Ventral striatum reactivity to reward and recent life stress interact to predict positive affect. Biological Psychiatry. 2012;72:157–163. doi: 10.1016/j.biopsych.2012.03.014. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Gee DG, Humphreys KL, Flannery J, Goff B, Telzer EH, Shapiro M, Hare TA, Bookheimer SY, Tottenham N. A developmental shift from positive to negative connectivity in human amygdala-prefrontal circuitry. Journal of Neuroscience. 2013;33:4584–4593. doi: 10.1523/JNEUROSCI.3446-12.2013. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 47. Gee DG, Gabard-Durnam LJ, Flannery J, Goff B, Humphreys KL, Telzer EH, Hare TA, Bookheimer SY, Tottenham N. Early developmental emergence of human amygdala-prefrontal connectivity after maternal deprivation. Proceedings of the National Academy of Sciences. 2013;110:15638–15643. doi: 10.1073/pnas.1307893110. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 48**. Herringa RJ, Burghy CA, Stodola DE, Fox ME, Davidson RJ, Essex MJ. Enhanced prefrontal-amygdala connectivity following childhood adversity as a protective mechanism against internalizing in adolescence. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. 2016;1:326–334. doi: 10.1016/j.bpsc.2016.03.003. Exposure to childhood adversity was associated with heightened amygdala reactivity to negative stimuli, but not positive stimuli, in late adolescence. Adolescents with low levels of internalizing symptoms following childhood adversity exhibited greater functional connectivity between the dorsal prefrontal cortex and amygdala in response to negative stimuli. Enhanced prefrontal regulation of amygdala reactivity may represent a protective factor for the development of internalizing psychopathology following exposure to adversity. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Dorsey S, McLaughlin KA, Kerns SEU, Harrison JP, Lambert HK, Briggs-King E, Cox JR, Amaya-Jackson L. Evidence Base Update for Psychosocial Treatments for Children and Adolescents Exposed to Traumatic Events. Journal of Clinical Child & Adolescent Psychology. doi: 10.1080/15374416.2016.1220309. in press. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 50. Berkowitz SJ, Stover CS, Marans SR. The child and family traumatic stress intervention: Secondary prevention for youth at risk of developing PTSD. Journal of Child Psychology and Psychiatry. 2011;52:676–685. doi: 10.1111/j.1469-7610.2010.02321.x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (199.9 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Annual Research Review: Rethinking childhood trauma-new research directions for measurement, study design and analytical strategies
Affiliations.
- 1 Social, Genetic and Developmental Psychiatry Centre, King's College London, London, UK.
- 2 Department of Child and Adolescent Psychiatry, Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK.
- 3 National and Specialist CAMHS Clinic for Trauma, Anxiety, and Depression, South London and Maudsley NHS Foundation Trust, London, UK.
- PMID: 31762042
- DOI: 10.1111/jcpp.13160
Childhood trauma is a key modifiable risk factor for psychopathology. Despite significant scientific advances, traumatised children still have poorer long-term outcomes than nontraumatised children. New research paradigms are, thus, needed. To this end, the review examines three dominant assumptions about measurement, design and analytical strategies. Current research warns against using prospective and retrospective measures of childhood trauma interchangeably; against interpreting cross-sectional differences in putative mediating mechanisms between adults with or without a history of childhood trauma as evidence of longitudinal changes from pre-trauma conditions; and against directly applying explanatory models of resilience or vulnerability to psychopathology in traumatised children to forecast individual risk in unseen cases. The warnings equally apply to research on broader measures of adverse childhood experiences (ACEs). Further research examining these assumptions can generate new insights on how to prevent childhood trauma and its detrimental effects.
Keywords: Childhood trauma; adverse childhood experiences; childhood abuse; childhood maltreatment; childhood victimization.
© 2019 Association for Child and Adolescent Mental Health.
Publication types
- Research Support, Non-U.S. Gov't
- Adverse Childhood Experiences*
- Child Abuse*
- Child, Preschool
- Neuropsychological Tests / standards*
- Psychological Trauma / diagnosis*
- Psychometrics / standards*
- Research Design / standards*
Grants and funding
- G1002190/MRC_/Medical Research Council/United Kingdom
- U24 AG047867/AG/NIA NIH HHS/United States
- DH_/Department of Health/United Kingdom
- P005918/MRC_/Medical Research Council/United Kingdom

IMAGES
COMMENTS
Gender differences influence the effect of childhood trauma on the HPA axis. Research involving men and women who were exposed to early trauma but who did not have any psychopathological diagnoses has shown stronger associations between trauma and increased CRF levels in men than in women .
Feb 1, 2022 · This article looks at the impact of childhood trauma on children's wellbeing and adult behavior from the perspective of 9 clinical professionals in Ireland. It exhibits how physical, sexual and emotional abuse disrupts one's life through analyzing coping strategies and behaviors adopted by childhood trauma victims following adversity exposure.
Aug 3, 2020 · A study by Harvard University found that children who experienced abuse or violence showed signs of early puberty, cellular aging and brain thinning. These findings suggest that trauma exposure may increase health risks later in life and highlight the need for early interventions.
Each domain of threat processing is associated with internalizing and externalizing psychopathology, as well as post-traumatic stress disorder (PTSD); although greater research is needed to clarify whether the specific disruptions in emotional learning associated with child trauma are associated with mental health problems other than ...
There is strong evidence of an association between childhood trauma and later mental illness. This association is particularly evident for exposure to bullying, emotional abuse, maltreatment and parental loss. The evidence suggests that childhood and adolescence are an important time for risk for la …
Results: We identified 22 childhood trauma cases (total score > 36) and, of the 89 non-childhood trauma cases, some individuals also experienced significant levels of trauma in one or more of the childhood trauma subtypes. Childhood trauma and some trauma subtypes were significantly correlated with a myriad of negative physiological and ...
This article discusses early childhood trauma and the negative long-term consequences that can cause life-long medical and psychological deficiencies. Early childhood trauma, especially complex trauma, can cause neurobiological changes that impact human development and cause significant changes in brain function. These changes in brain structures are responsible for cognitive and physical ...
Nov 30, 2016 · PDF | On Nov 30, 2016, Shannon Eaton Allen published Childhood Trauma: A Comprehensive Review of Effects, Assessments, and Treatments | Find, read and cite all the research you need on ResearchGate
Childhood trauma is a key modifiable risk factor for psychopathology. Despite significant scientific advances, traumatised children still have poorer long-term outcomes than nontraumatised children. New research paradigms are, thus, needed. To this end, the review examines three dominant assumptions …
Mar 15, 2021 · Childhood trauma (CT) is one of the most robust and significant risk factors for depressive and anxiety disorders. CT is commonly defined as "all forms of physical and/or emotional ill-treatment, sexual abuse, neglect or negligent treatment or commercial or other exploitation, resulting in actual or potential harm to the child's health, survival, development or dignity in the context of a ...