- Search by keyword
- Search by citation
Page 1 of 63

Application of three-dimensional visualization technology in early surgical repair of bile duct injury during laparoscopic cholecystectomy
This study aimed to explore the application value of three-dimensional (3D) visualization technology in the early surgical repair of bile duct injury during laparoscopic cholecystectomy (LC).
- View Full Text
Risk factors and distribution pattern of lateral lymph node recurrence after central neck dissection for cN1a papillary thyroid carcinoma
The indication and extent of selective lateral neck dissection (LND) for cN1a papillary thyroid carcinoma (PTC) remain uncertain. The present study aimed to identify potential predictors and distribution patte...
Whether T-tube biliary drainage is necessary after pancreaticoduodenectomy: a single-center retrospective study
Postoperative complications of pancreaticoduodenectomy (PD) are still a thorny problem. This study aims to verify the preventative impact of T-tube on them.
Observations from the first 100 cases of intraoperative MRI – experiences, trends and short-term outcomes
We sought to analyze, in well-defined clinical setting, the first 100 patients treated at the intraoperative MRI (iMRI) hybrid surgical theatre at our facility in a population-based setting to evaluate which p...
Postoperative early laboratory changes and follow-up process of patients underwent hyperthermic intrathoracic chemotherapy
The aim of combining hyperthermic intrathoracic chemotherapy (HITHOC) with surgery is to achieve local control in patients with pleural malignancies. Liver and kidney dysfunction resulting from this procedure ...
Short-term safety and effectiveness of conversion from sleeve gastrectomy to Ring augmented Roux-en-Y gastric bypass
Weight recurrence, suboptimal clinical response and functional disorder (such as reflux) after a Sleeve Gastrectomy (SG) are problems that may require conversional surgery. For reflux, conversion to Roux-en-Y ...
Orthostatic intolerance during early mobilization following thoracoscopic lung resection: a prospective observational study
Early postoperative mobilization is important for enhanced recovery but can be hindered by orthostatic intolerance. However, study on postoperative orthostatic intolerance in thoracoscopic lung resection is li...
Hypoparathyroidism after total thyroidectomy: reactive to symptoms supplementation
After total thyroidectomy (TT), postoperative hypoparathyroidism (PH) is the most frequent complication. Yet, management strategies for PH remain disputed. The aim of this study was to evaluate outcomes of a r...
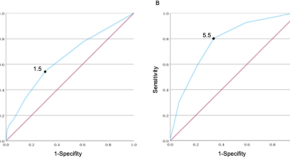
Assessing the accuracy of the revised Cardiac Risk Index compared to the American Society of Anaesthesiologists physical status classification in predicting Pulmonary and Cardiac complications among non-cardiothoracic surgery patients at Muhimbili National Hospital: a prospective cohort study
The Revised Cardiac Risk Index (RCRI) and the American Society of Anaesthesiologists (ASA-PS) classification system are two commonly used tools for preoperative risk assessment. This study aimed to assess the ...
Treatment outcome and associated factors of infantile hypertrophic pyloric stenosis at eastern Ethiopia public hospitals
Infantile hypertrophic pyloric stenosis (IHPS) is a condition whose etiology is not clear, but it is characterized by progressive hypertrophy of the circular muscles of the pylorus with consequent obstruction ...
Indocyanine green fluorescence in the evaluation of post-resection pancreatic remnant perfusion after a pancreaticoduodenectomy: a clinical study protocol
Pancreaticoduodenectomy is associated with an incidence of postoperative complications of approximately 41%. One of the most severe complications is a postoperative pancreatic fistula. The exact cause of posto...
Predictive factors for intrathoracic anastomotic leakage and postoperative mortality after esophageal cancer resection
Esophageal cancer is currently one of the high-risk malignant tumors worldwide, posing a serious threat to human health. This study aimed to analyse the causes of postoperative mortality and intrathoracic anas...
Efficacy of thoracic endovascular aortic repair versus medical therapy for treatment of type B aortic dissection
Techniques in endovascular therapy have evolved to offer a promising alternative to medical therapy alone for Type B aortic dissections (TBADs).
Laparoscopic Sugarbaker repair of parastomal hernia following radical cystectomy and ileal conduit: a single-center experience
Parastomal hernia (PH) is a frequent complication following radical cystectomy and ileal conduit. The purpose of this study was to summarize the clinical experience and technical characteristics of laparoscopi...
When the first try fails: re-implementation of SIMPL in a general surgery residency
Workplace-based assessment (WBA) can facilitate evaluation of operative performance; however, implementation of WBA is sometimes unsuccessful. The American Board of Surgery Entrustable Professional Activities ...
Risk factors for deep vein thrombosis of the lower extremity after total hip arthroplasty
To investigate the risk factors for deep vein thrombosis (DVT) following total hip arthroplasty (THA).
Progress, challenges, and future perspectives of robot-assisted natural orifice specimen extraction surgery for colorectal cancer: a review
With the continuous advancements in precision medicine and the relentless pursuit of minimally invasive techniques, Natural Orifice Specimen Extraction Surgery (NOSES) has emerged. Compared to traditional surg...
Oncological outcomes of minimally invasive surgery in non-endometrioid endometrial Cancer patients with varying prognostic risks: a retrospective cohort study based on the ESGO/ESTRO/ESP 2020 guidelines
Non-endometrioid endometrial carcinomas (NEEC) are characterized by their rarity and adverse prognoses. This study evaluates the outcomes of open versus minimally invasive surgery (MIS) in NEEC patients strati...
Assessing the impact of enhanced hygiene precautions during the COVID-19 pandemic on surgical site infection risk in abdominal surgeries
A surgical site infection (SSI) is a postoperative infection that occurs at or near the surgical incision. SSIs significantly increase morbidity, mortality, length of hospital stay, and healthcare costs. The W...
Role of subcutaneous closed suction drain in the prevention of incisional surgical site infection after loop ileostomy reversal with purse-string skin closure: a retrospective observational study
Surgical site infection (SSI) is not rare after loop ileostomy reversal. This study assessed the effects of a subcutaneous closed suction drain on reducing SSIs after loop ileostomy reversal with purse-string ...
Fournier’s Gangrene: clinical case review and analysis of risk factors for mortality
Fournier’s Gangrene is a severe surgical infectious disease, and various risk factors can increase its mortality rate. The purpose of this study is to retrospectively analyze the clinical characteristics and l...
Patterns, treatment outcome and associated factors of surgically treated thyroid disease at public hospitals in Eastern Ethiopia: a retrospective cross-sectional study
Thyroid disease is a global health problem and the most common type of endocrine disorder next to diabetic mellitus, accounting for around 30–40% burden of the endocrine disorders.
Robotic purse-string suture technique for intracorporeal anastomosis using double-stapling technique in robotic resection of rectal and sigmoid colon cancer: a propensity score-matched analysis
Robotic three-dimensional magnified visual effects and field of view stabilization have enabled precise surgical operations. Intracorporeal anastomosis in right-sided colorectal cancer surgery is expected to s...
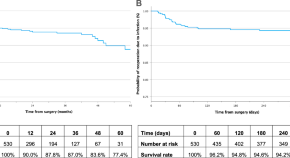
Liver resection for hepatocellular carcinoma in elderly patients: does age matter?
Evaluation of the influence of the age of the patients upon the outcomes of liver resection (LR) for hepatocellular carcinoma (HCC).
Comparison of efficacy and safety of different suction pressure for speeding non-ventilated lung collapse in uniport video-assisted thoracoscopic surgery: a randomized-controlled trial
The bronchial suction has been applied in speeding lung collapse. Low suction pressure may not speed lung collapse, but high pressure causes occult lung injury. The aim of the study was to explore efficacy and...
Reduced port laparoscopic rectopexy for full-thickness rectal prolapse
Laparoscopic rectopexy is an established treatment option for full-thickness rectal prolapse. Recently, reduced port surgery (RPS) has emerged as a novel concept, offering reduced postoperative pain and improv...
Early post-operative outcome of pre-pectoral implant-based immediate total breast reconstruction with Polyglactin 910 (Vicryl™) mesh – low cost solution for a low-middle income country
The incidence of breast cancer in Pakistan has been rising with approximately one third of these patients requiring mastectomy. Among breast reconstruction treatment options, the use of Acellular Dermal Matrix...
Umbilical double-port laparoscopy combined with extraperitoneal water injection for the treatment of giant inguinal hernias in infants and young children
Exploration of the efficacy of treating large indirect inguinal hernias in infants and young children using umbilical double-port laparoscopy combined with extraperitoneal water injection.
Let’s talk about the surgeon well-being
Safety and efficacy of bilateral superselective adrenal arterial embolization for treatment of idiopathic hyperaldosteronism: a prospective single-center study.
This study aimed to assess the efficacy and safety of bilateral superselective adrenal arterial embolization (SAAE) in patients with bilateral idiopathic hyperaldosteronism (IHA), a subtype of PA.
Total laparoscopic radical resection of hilar cholangiocarcinoma: preliminary experience of a single center
The aim of this study was to describe our preliminary experience in the procedure of laparoscopic radical resection of hilar cholangiocarcinoma and to evaluate its feasibility, safety, and clinical efficacy.
The effects of remimazolam in combination with estazolam on postoperative hemodynamics and pain intensity in patients undergoing laparoscopic gastrointestinal surgery
This study aimed to investigate the effects of combining remimazolam with estazolam on hemodynamics and pain levels after laparoscopic gastrointestinal surgery.
The safety of not implementing endoscopic nasobiliary drainage after elective clearance of choledocholithiasis: a systematic review and meta-analysis
Endoscopic nasobiliary drainage (ENBD) is used as a drainage technique in patients with choledocholithiasis after stone removal. However, ENBD can cause discomfort, displacement, and other complications. This ...
Meta-analysis of robotic-assisted NOSE versus traditional TWSR in colorectal cancer surgery: postoperative outcomes and efficacy
This meta-analysis aimed to assess the safety and efficacy of robotic-assisted natural orifice specimen extraction surgery (NOSE) compared to traditional robotic transabdominal wall specimen retrieval surgery ...
Study protocol of the FRENCH24-ANIS study: postoperative anti-infective strategy following pancreaticoduodenectomy in patients with preoperative biliary stents—an intergroup FRENCH-ACHBT-SFAR prospective randomized controlled trial
Despite advances in surgical techniques and care, pancreatoduodenectomy (PD) continues to have high morbidity and mortality rates. Complications such as sepsis, hemorrhage, pulmonary issues, shock, and pancrea...
Comparative study on three-dimensional versus two-dimensional imaging using a computer-assisted surgery system for preoperative planning in pediatric middle hepatic tumors
The study objective was to compare three-dimensional and two-dimensional imaging using computer-assisted systems (CASs) in clinical guidance for preoperative surgical planning for middle hepatic tumors in chil...
Research progress on bariatric surgery for hyperuricemia
Hyperuricemia is closely linked to obesity. As lifestyles and dietary patterns evolve, the prevalence of hyperuricemia has been on the rise. Bariatric surgery, an efficacious intervention for morbid obesity an...
Primary schwannoma of the thyroid gland: analysis of case characteristics and review of the literature
To improve the characteristics of primary thyroid schwannomas (PTS) and to provide reference basis for clinical diagnosis and treatment.
Risk factors of textbook outcome in laparoscopic pancreatoduodenectomy: results from a prospective high-volume center study
Achieving textbook outcome (TO) implies a smooth recovery post-operation without specified composite complications. This study aimed to evaluate TO in laparoscopic pancreaticoduodenectomy (LPD) and identify in...
A new gap balancing technique with functional alignment in total knee arthroplasty using the MAKO robotic arm system: a preliminary study
Gap tension is an important factor influencing the clinical outcomes of total knee arthroplasty (TKA). Traditional mechanical alignment (MA) places importance on neutral alignment and often requires additional...
Anatomical observations on 30 cadavers: new insights into the relationship between the posterior wall of the inguinal canal and the cremaster
Clarify the composition of the Posterior wall of the Inguinal Canal(PWIC), the location and composition of the Transverse Fascia(TF), and the tissue origin of the Cremaster(C) by observing the anatomy of the i...
Partial (incomplete) removal of granulation tissue using modified minimally invasive surgical technique in treatment of infrabony defects (randomized control clinical trial)
This study aims to compare the clinical and radiographic outcomes after complete versus incomplete removal of granulation tissue (GT) during modified minimally invasive surgical technique (M-MIST) for manageme...
Early postoperative fever as a predictor of pancreatic fistula after pancreaticoduodenectomy: a single-center retrospective observational study
The connection between early postoperative fever and clinically relevant postoperative pancreatic fistula (CR-POPF) after pancreaticoduodenectomy remains unclear. This study aimed to investigate this associati...
Opioid-free anesthesia with esketamine-dexmedetomidine versus opioid-based anesthesia with propofol-remifentanil in shoulder arthroscopy: a randomized controlled trial
OFA (Opioid-free anesthesia) has the potential to reduce the occurrence of opioid-related adverse events and enhance postoperative recovery. Our research aimed to investigate whether OFA, combining esketamine ...
Virus and viral components transmitted through surgical smoke; a silent danger in operating room: a systematic review
During surgical procedures, heat-generating devices are widely used producing surgical smoke (SS). Since the SS can transmit infectious viruses, this systematic review was designed to investigate the potential...
Factors predicting the use of the backward upward rightward pressure maneuver in thyroid surgery: a single-center retrospective cohort study
The purpose of this study was to evaluate the predictability of utilizing the backward upward rightward pressure (BURP) maneuver and the efficacy of related tests in patients with a challenging airway and a Ma...
The effect of high-volume intraoperative fluid administration on outcomes among pediatric patients undergoing living donor liver transplantation
Pediatric patients undergoing liver transplantation are particularly susceptible to complications arising from intraoperative fluid management strategies. Conventional liberal fluid administration has been cha...
Rescue liver transplantation for post-hepatectomy liver failure- single center retrospective analysis
Liver transplantation (LT) is a well-established method applied for the treatment of various liver diseases, including primary and secondary malignancies, as well as acute liver failure triggered by different ...
Surgical management of pancreatic cancer in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: a 5 years retrospective descriptive study
The incidence of Pancreatic cancer is different in different parts of the world. It is a cancer with the worst prognosis of all malignancies. Pancreatic cancer is predominantly a disease of an older population...
Invasive treatment for extracranial carotid artery aneurysm: a single-center case series and literature review
Extracranial carotid artery aneurysm (ECAA) is a rare peripheral arterial disease. The main treatment strategies include conservative treatment, open surgery, endovascular treatment, and hybrid techniques, and...
Important information
Editorial board
For authors
For editorial board members
For reviewers
- Manuscript editing services
Annual Journal Metrics
Citation Impact 2023 Journal Impact Factor: 1.6 5-year Journal Impact Factor: 1.9 Source Normalized Impact per Paper (SNIP): 1.019 SCImago Journal Rank (SJR): 0.520 Speed 2023 Submission to first editorial decision (median days): 21 Submission to acceptance (median days): 131 Usage 2023 Downloads: 1,809,339 Altmetric mentions: 257
Peer-review Terminology
The following summary describes the peer review process for this journal:
Identity transparency: Single anonymized
Reviewer interacts with: Editor
Review information published: Review reports. Reviewer Identities reviewer opt in. Author/reviewer communication
More information is available here
- Follow us on Twitter
BMC Surgery
ISSN: 1471-2482
- General enquiries: [email protected]

- Weill Cornell Medicine

Research Areas
As part of one the most prestigious academic medical centers in the country, the Department of Surgery at Weill Cornell Medicine undertakes a wide breadth of research each year and participates in both intramural and extramural collaborations.
The research areas highlighted below are just a few of topics we are actively studying. They are comprised of several high-priority programs represented by departmental laboratories dedicated to translational science so that patients can receive the best care possible.
Cancer Research
Critical care and trauma, metabolism and diabetes, stem cell biology and regenerative medicine, surgical innovation, transplant biology, vascular biology, wound healing, outcome research, find a physician.
Visit our Surgery YouTube channel to view our video library.
Navigation group
Submission open
- Submission closed
- All sections
- Cardiovascular Surgery
- Colorectal and Proctological Surgery
- Genitourinary Surgery
- Neurosurgery
- Obstetrics and Gynecological Surgery
- Orthopedic Surgery
- Otorhinolaryngology - Head and Neck Surgery
- Pediatric Orthopedics
- Pediatric Surgery
- Pediatric Urology
- Reconstructive and Plastic Surgery
- Surgical Oncology
- Thoracic Surgery
- Vascular Surgery
- Visceral Surgery
- All results
- Has no e-book
Research Topics

Multidisciplinary Insights into Distal Tibiofibular Joint Injuries: An Integrative Analysis of Surgical Techniques, Rehabilitation Protocols, and Podiatric Interventions
- Roberto Tedeschi
- Danilo Donati
- Daniela Platano
Minimally Invasive Treatments for Lumbar Spine Disorders
- Osvaldo Mazza
Clinical Application of Telemedicine for Postoperative Rehabilitation and Conservative Treatment in Orthopaedics
Cholesteatoma surgery: treatment outcome and follow up.
- Hans Thomeer
- Nicolas Verhaert
- Marc Lammers
- Paul Merkus
- 1,299 views
Microflora and Bacterial Translocation in Intestinal Obstruction
- Zhandos Muratovich Koishibayev
- Leila Meiramovna Koishibayeva
- Tomas Poskus
- Gabriel Sandblom

Optimizing Outcomes in Pelvic Exenteration Surgery for Advanced Pelvic Malignancies
- Richard Garfinkle
- William Perry
- Kilian Brown
Implementing Risk Prediction Models to Enhance Clinical Outcomes in Orthopaedics and Arthroplasty
- Daniel Gould
- Sharm Thuraisingam
Recent Advances and New Challenges in Minimally Invasive Surgery and Chemotherapy for Colorectal Cancer-volume 2
- Hiroki Hashida
- Nobu OSHIMA
Current Advances in the Understanding and Management of Pelvic Organ Prolapse
- Yonghong Lin
- Carlo Ronsini

Innovations and Challenges in Surgical Education
- Stefano Cianci
- Marco Scarci
- Gaetano Gallo
- Stavros K. Kakkos
- Philipp Taussky
- Mounir J. Haurani
- 2,985 views
10th Anniversary of Frontiers in Surgery: Celebrating Progress and Envisioning the Future of Multidisciplinary Surgery
- Dennis Paul Orgill
- Robert James Cerfolio
- Małgorzata Wierzbicka

Surgical Approaches and Outcomes in Cervical and Thoracic Myelopathies
- Georges Naim ABI LAHOUD
- Moussa Antoine Chalah
- Samar S. Ayache
Surgical Revascularization of the Ischemic Myocardium in the third millennium
- Antonio Maria Calafiore
- Gianni Angelini

Progress of New Technologies in Gastric Cancer Minimally Invasive Treatments
- Kazutaka Obama
- Xianquan Zhan

The Application of EUS-FNA in the Diagnosis of Pancreatic Cancer
- Giovanni Marchegiani
- 1,305 views
Transformation and Clinical Application of Innovative Medical Devices Related to Neuroscience
- Xuejian Wang
- Nicola Montemurro
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
Surgery articles from across Nature Portfolio
Surgery is a procedure in which incision and physical manipulation are used to treat a patient with an injury or a disease. The patient's tissues are cut during this technique to permit the manipulation of tissues that are otherwise inaccessible.
Related Subjects
- Bariatric surgery
- Colorectal surgery
- Fistula creation
- Neurosurgery
- Reconstruction
- Surgical oncology
- Transplantation
Latest Research and Reviews
Surgical Apgar Score and Controlling Nutritional Status Score can be predictors of major postoperative complications after spine surgery
- Takahiro Sunami
- Kousei Miura
- Masashi Yamazaki
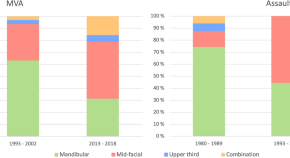
Paediatric maxillofacial fractures have increased in incidence and their nature and aetiology have changed during three decades
- Aura Kirvelä
- Anna Liisa Suominen
- Hanna Thorén
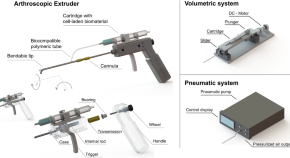
Arthroscopic device with bendable tip for the controlled extrusion of hydrogels on cartilage defects
- Daniele Guarnera
- Francesco Restaino
- Leonardo Ricotti
Risk factors for reoperation of inflatable penile prosthesis among an ethnically diverse urban population in a high-volume center
- Noah Hawks-Ladds
- Mustufa Babar
- Pedro Maria
Can AI chatbots accurately answer patient questions regarding vasectomies?
- Edwin Mouhawasse
- Christopher W. Haff
- Justin M. Dubin
Prioritising patients for publicly funded bariatric surgery in Queensland, Australia
- Paul Scuffham
- Megan Cross
- Jody Paxton
News and Comment
Vitrectomy for vitreous haemorrhage due to proliferative diabetic retinopathy in eyes with mild visual impairment
- Rodrigo Anguita
- Louisa Wickam
Response to Comment on: Patient out-of-pocket costs for guideline-recommended treatments for erectile dysfunction: a medicare cost modeling analysis
- Darshan P. Patel
- Tung-Chin Hsieh

TEER is non-inferior to surgery in patients with secondary mitral regurgitation
In patients with heart failure and secondary mitral valve regurgitation, transcatheter edge-to-edge repair is non-inferior to mitral valve surgery with respect to a composite of death, hospitalization for heart failure, reintervention, implantation of an assist device or stroke at 1 year after the procedure, according to findings from the MATTERHORN trial.
- Irene Fernández-Ruiz

Response to comment on: bioengineered dermal matrix (Integra®) reduces donor site morbidity in total phallic construction with radial artery forearm free-flap
- Marco Falcone
- Federica Peretti
- Lorenzo Cirigliano
A model for anterior vitrectomy in real patients: is it safe, ethical and necessary?
- Georgios D. Panos
- Alexander Foss
- Harminder Dua
Tertiary lymphoid organs contribute to kidney allograft rejection
- Ellen F. Carney
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Recent advances:...
Recent advances: General surgery
- Related content
- Peer review
- Carlos U Corvera , resident in general surgery a ,
- Kimberly S Kirkwood , assistant professor of surgery ([email protected]) a
- a University of California, San Francisco, Department of Surgery, Room U-372, 533 Parnassus Avenue, San Francisco, CA 94143-0790, USA
- Correspondence to: Dr Kirkwood
Introduction
In the modern era of managed care, surgeons have been pressured to re-evaluate the management of many common disease processes and seek cost effective measures while maintaining the quality of patient care. Recent advances in anaesthesia and minimal access surgery have facilitated the remarkable expansion of ambulatory or “short stay” surgery. As a result, patients with gall stones, gastro-oesophageal reflux, and peptic ulcers now have less morbidity and shorter hospital stays.
The topics in this article were selected after we conducted an informal survey among the general surgeons at our institution. The consensus was that these topics, which have been influenced by managed care and advancing technology, represent the most recent and ongoing changes in general surgery. A Medline search for the topic ambulatory surgery used the keywords “ambulatory surgery,” “postoperative nausea and vomiting,” “propofol,” and “preemptive analgesia.” The keywords in the search for minimal access surgery were “laparoscopic common bile duct exploration,” “reflux disease,” “laparoscopic fundoplication,” “pancreatic pseudocyst,” and “perforated duodenal ulcer.” Additional keywords included “surgical treatment” and “laparoscopic and minimally invasive surgery.” Articles published since 1995 formed the basis of this review.
Ambulatory surgery
Ambulatory surgery was introduced in 1970, and its widespread acceptance was influenced by patients, surgeons, and cost considerations. Today, the growth of outpatient surgery is fuelled by a healthcare industry that demands high quality care at a lower cost. The current competitive healthcare environment has exerted tremendous pressure on surgeons and hospitals to increase the number and variety of outpatient procedures. It has been estimated that by the year 2000, about 75% of all surgical procedures in the United States will be ambulatory procedures. 1 The recent successful expansion of outpatient surgery is predicated on advances in anaesthesia and a sweeping acceptance of minimally invasive techniques.
The most common reasons for patients to require admission after …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
Navigating Surgical Challenges: Updates in General Surgery Techniques and Strategies
- January 2021

- Japan Clinical Research Support Unit

- L. D. College of Engineering
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
General Surgery: Current Trends and Recent Innovations
Cite this chapter.

- John P. Cullen 3 &
- Mark A. Talamini 4
2981 Accesses
2 Citations
In surgery, new technology has been developed to eliminate some problems that surgeons face during more challenging laparoscopic or conventional operations. Surgical robotic systems have restored much of what was lost and altered the learning curve in the surgeon's favor. At the same time, advanced surgical instruments and optics continue the trend of the smaller scar. Minimally invasive surgery has given birth to a new and exciting era in surgical research. The future of surgical research lies, in part, in computer and visual technology.
This chapter begins by describing many of the current trends in surgical research. The second half of the chapter describes the latest innovations in general surgical research. Surgeons in numerous disciplines continue to make great strides in basic science research. However, the latest and most exciting innovations have largely developed through the integration of new innovative technology into surgical practice.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others

The Origins of Minimally Invasive and Robotic Surgery and Their Impact on Surgical Practice: A Sociological, Technological History

Basic Setup, Principles, and Troubleshooting in Robotic Surgery

Robotic Applications in Advancing General Surgery
Kohn LT, Corrigan JM, Donaldson MS (2000) To err is human: building a safer health system. National Academy Press, Washington
Google Scholar
Bates DW, Leape LL, Cullen DJ et al (1998) Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 280:1311–1316
Article PubMed CAS Google Scholar
Anon (2003) Scanning medication barcodes improves accuracy at Lehigh Valley Hospital. Perform Improv Advis 7:132–134; 129
Harvey-Berino J, Pintauro S, Buzzell P et al (2004) Effect of internet support on the long-term maintenance of weight loss. Obes Res 12:320–329
Article PubMed Google Scholar
Polzien KM, Jakicic JM, Tate DF et al (2007) The efficacy of a technology-based system in a short-term behavioral weight loss intervention. Obesity (Silver Spring) 15:825–830
Article Google Scholar
Saperstein SL, Atkinson NL, Gold RS (2007) The impact of Internet use for weight loss. Obes Rev 8:459–465
Irwin RS (2007) Clinical trial registration promotes patient protection and benefit, advances the trust of everyone, and is required. Chest 131:639–641
Khuri SF, Daley J, Henderson W et al (1998) The Department of Veterans Affairs' NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg 228:491–507
Silverman H, Hull SC, Sugarman J (2001) Variability among institutional review boards' decisions within the context of a multicenter trial. Crit Care Med 29:235–241
Dyrbye LN, Thomas MR, Mechaber AJ et al (2007) Medical education research and IRB review: an analysis and comparison of the IRB review process at six institutions. Acad Med 82:654–660
Stair TO, Reed CR, Radeos MS et al (2001) Variation in institutional review board responses to a standard protocol for a multicenter clinical trial. Acad Emerg Med 8:636–641
Kilbridge P (2003) The cost of HIPAA compliance. N Engl J Med 348:1423–1424
O'Herrin JK, Fost N, Kudsk KA (2004) Health Insurance Portability Accountability Act (HIPAA) regulations: effect on medical record research. Ann Surg 239:772–776; discussion 776–778
Kulynych J, Korn D (2002) The effect of the new federal medical-privacy rule on research. N Engl J Med 346:201–204
Tovino SA (2004) The use and disclosure of protected health information for research under the HIPAA privacy rule: unrealized patient autonomy and burdensome government regulation. S D Law Rev 49:447–502
PubMed Google Scholar
Henke PK, Fewel M (2007) Surgical research and the new privacy laws. Bull Am Coll Surg 92:26–29
Dunlop AL, Graham T, Leroy Z et al (2007) The impact of HIPAA authorization on willingness to participate in clinical research. Ann Epidemiol 17:899–905
Harrison RW III (2001) Impact of biomedical research on African Americans. J Natl Med Assoc 93:6S–7S
Jackson HH, Jackson JD, Mulvihill SJ et al (2004) Trends in research support and productivity in the changing environment of academic surgery. J Surg Res 116:197–201
Avis FP, Ellenberg S, Friedman MA (1988) Surgical oncology research. A disappointing status report. Ann Surg 207:262–266
Bland KI (2007) Concerning trends and outcomes for National Institutes of Health funding of cancer research. J Surg Oncol 95:161–166
Mello MM, Clarridge BR, Studdert DM (2005) Academic medical centers' standards for clinical-trial agreements with industry. N Engl J Med 352:2202–2210
Kaiser J (2007) Conflict of interest. Stung by controversy, biomedical groups urge consistent guidelines. Science 317:441
Marescaux J, Leroy J, Rubino F et al (2002) Transcontinental robot-assisted remote telesurgery: feasibility and potential applications. Ann Surg 235:487–492
Pasticier G, Rietbergen JB, Guillonneau B et al (2001) Robotically assisted laparoscopic radical prostatectomy: feasibility study in men. Eur Urol 40:70–74
Patel VR, Chammas MF Jr, Shah S (2007) Robotic assisted laparoscopic radical prostatectomy: a review of the current state of affairs. Int J Clin Pract 61:309–314
Menon M, Kaul S, Bhandari A et al (2005) Potency following robotic radical prostatectomy: a questionnaire based analysis of outcomes after conventional nerve sparing and prostatic fascia sparing techniques. J Urol 174:2291–2296; discussion 2296
Talamini MA, Chapman S, Horgan S et al (2003) A prospective analysis of 211 robotic-assisted surgical procedures. Surg Endosc 17:1521–1524
Melvin WS, Dundon JM, Talamini M et al (2005) Computer-enhanced robotic telesurgery minimizes esophageal perforation during Heller myotomy. Surgery 138:553–558; discussion 558–559
Galvani C, Gorodner MV, Moser F et al (2006) Laparoscopic Heller myotomy for achalasia facilitated by robotic assistance. Surg Endosc 20:1105–1112
Moser F, Horgan S (2004) Robotically assisted bariatric surgery. Am J Surg 188:38S–44S
Yu SC, Clapp BL, Lee MJ et al (2006) Robotic assistance provides excellent outcomes during the learning curve for laparoscopic Roux-en-Y gastric bypass: results from 100 robotic-assisted gastric bypasses. Am J Surg 192:746–749
Mohr CJ, Nadzam GS, Curet MJ (2005) Totally robotic Roux-en-Y gastric bypass. Arch Surg 140:779–786
Kendoff D, Pearle A, Hufner T et al (2007) First clinical results and consequences of intraoperative three-dimensional imaging at tibial plateau fractures. J Trauma 63:239–244
Nathan CO, Chakradeo V, Malhotra K et al (2006) The voice-controlled robotic assist scope holder AESOP for the endoscopic approach to the sella. Skull Base 16:123–131
Nebot PB, Jain Y, Haylett K et al (2003) Comparison of task performance of the camera-holder robots EndoAssist and Aesop. Surg Laparosc Endosc Percutan Tech 13:334–338
Husted TL, Broderick TJ (2006) NASA and the emergence of new surgical technologies. J Surg Res 132:13–16
Rentschler ME, Dumpert J, Platt SR et al (2007) Natural orifice surgery with an endoluminal mobile robot. Surg Endosc 21:1212–1215
Kalloo AN, Singh VK, Jagannath SB et al (2004) Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc 60:114–117
Rattner D, Kalloo A (2006) ASGE/SAGES Working Group on Natural Orifice Translumenal Endoscopic Surgery. October 2005. Surg Endosc 20:329–333
Pai RD, Fong DG, Bundga ME et al (2006) Transcolonic endoscopic cholecystectomy: a NOTES survival study in a porcine model (with video). Gastrointest Endosc 64:428–434
Park PO, Bergstrom M, Ikeda K et al (2005) Experimental studies of transgastric gallbladder surgery: cholecystectomy and cholecystogastric anastomosis (videos). Gastrointest Endosc 61:601–606
Jagannath SB, Kantsevoy SV, Vaughn CA et al (2005) Peroral transgastric endoscopic ligation of fallopian tubes with long-term survival in a porcine model. Gastrointest Endosc 61:449–453
Bergstrom M, Ikeda K, Swain P et al (2006) Transgastric anastomosis by using flexible endoscopy in a porcine model (with video). Gastrointest Endosc 63:307–312
Swain P (2007) The ShapeLock system adapted to intragas-tric and transgastric surgery. Endoscopy 39:466–470
Schweitzer M (2004) Endoscopic intraluminal suture plication of the gastric pouch and stoma in postoperative Roux-en-Y gastric bypass patients. J Laparoendosc Adv Surg Tech A 14:223–226
van Noordwijk J (2001) Dialysing for life: the development of the artificial kidney. Kluwer, Boston
Book Google Scholar
Wolff B, Machill K, Schumacher D et al (2007) MARS dialysis in decompensated alcoholic liver disease: a single-center experience. Liver Transpl 13:1189–1192
Kjaergard LL, Liu J, Als-Nielsen B et al (2003) Artificial and bioartificial support systems for acute and acute-on-chronic liver failure: a systematic review. JAMA 289:217–222
Sen S, Williams R, Jalan R (2005) Emerging indications for albumin dialysis. Am J Gastroenterol 100:468–475
Gray NA Jr, Selzman CH (2006) Current status of the total artificial heart. Am Heart J 152:4–10
Leprince P, Bonnet N, Rama A et al (2003) Bridge to transplantation with the Jarvik-7 (CardioWest) total artificial heart: a single-center 15-year experience. J Heart Lung Transplant 22:1296–1303
Jordan SW, Chaikof EL (2007) Novel thromboresistant materials. J Vasc Surg 45(Suppl A):A104–A115
Cobb WS, Kercher KW, Heniford BT (2005) The argument for lightweight polypropylene mesh in hernia repair. Surg Innov 12:63–69
Ren CJ, Fielding GA (2003) Laparoscopic adjustable gastric banding [Lap-Band]. Curr Surg 60:30–33
McNatt SS, Longhi JJ, Goldman CD et al (2007) Surgery for obesity: a review of the current state of the art and future directions. J Gastrointest Surg 11:377–397
Steiner S, Dyer N, Everett J et al (2005) Will we merge with machines? Available at: http://www.popsci.com/scitech/article/2005-08/will-we-merge-machines
Ahlberg G, Heikkinen T, Iselius L et al (2002) Does training in a virtual reality simulator improve surgical performance? Surg Endosc 16:126–129
Hanly EJ, Miller BE, Kumar R et al (2006) Mentoring console improves collaboration and teaching in surgical robotics. J Laparoendosc Adv Surg Tech A 16:445–451
Cubano M, Poulose BK, Talamini MA et al (1999) Long distance telementoring. A novel tool for laparoscopy aboard the USS Abraham Lincoln. Surg Endosc 13:673–678
Download references
Author information
Authors and affiliations.
Department of Surgery, University of California at San Diego, 200 West Arbor Drive, San Diego, CA, 8400, USA
John P. Cullen
Department of Surgery, University of California at San Diego, 200 West Arbor Drive, #8400, San Diego, CA, 92103, USA
Mark A. Talamini
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mark A. Talamini .
Editor information
Editors and affiliations.
Dept. Biosurgery & Surgical Technology, Imperial College London St. Mary's Hospital London, 10th floor QEQM Bldg. Praed Street, London, W2 1NY, United Kingdom
Thanos Athanasiou & Ara Darzi &
UCSF Global Health Sciences, 3333 California Street, Suite 285, San Francisco L, CA, 94143-0443, USA
Haile Debas
Rights and permissions
Reprints and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cullen, J.P., Talamini, M.A. (2010). General Surgery: Current Trends and Recent Innovations. In: Athanasiou, T., Debas, H., Darzi, A. (eds) Key Topics in Surgical Research and Methodology. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-71915-1_62
Download citation
DOI : https://doi.org/10.1007/978-3-540-71915-1_62
Publisher Name : Springer, Berlin, Heidelberg
Print ISBN : 978-3-540-71914-4
Online ISBN : 978-3-540-71915-1
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Research: Innovations and Advancements from the Department of Surgery
The practice of surgery at Johns Hopkins is grounded in research. Our investigations drive innovations in surgical technique and patient safety, advance in the understanding and treatment of disease and trauma, and develop new technologies to help individuals and populations. We seek to further knowledge and perfect practice both in our own community and around the world.
Developing better, safer and novel approaches is part of our historical legacy and ongoing mission. From the groundbreaking contributions in infection control, use of anesthesia and surgical treatment of breast cancer from our first surgeon-in-chief, William Halsted; through the lifesaving “Blue Baby” procedure for children born with congenital heart defects developed by Helen Taussig, Vivien Thomas and Alfred Blalock; to today’s work in minimally invasive robotic surgery and transplant techniques, our work has continually improved the experience and outcomes for patients both within our wards and around the world.
Members of the department pursue investigations in areas ranging from cancer epigenetics to vascular repair. We are tackling some of the most difficult and lethal diseases, including melanoma, gastric cancer and pancreatic cancer. We seek to nurture the next generation of leaders through our residencies, fellowships and collaborations with other researchers across a variety of disciplines to develop innovations such as bionic limbs and a radically new artificial heart .
We invite you to learn more about the work we do:
- Learn about our work in outcomes research at JSCOR.org
- Read the latest issue of Johns Hopkins Surgery
- Search clinical trials in cancer treatment at the Kimmel Cancer Center
- Search all clinical trials at the Johns Hopkins Institute for Clinical and Translational Research
- Advance our work by learning about ways to give
- See us on twitter
- See us on facebook
- See us on youtube
- See us on instagram
General Surgery Research Initiatives

Asian Liver Center
The Asian Liver Center at Stanford University is the first non-profit organization in the United States that addresses the disproportionately high rates of chronic hepatitis B infection and liver cancer in Asians and Asian Americans. Founded in 1996, the center addresses the gaps in the fight against hepatitis B through a four-pronged approach of collaboration, advocacy, research, and education & outreach (CARE). The ultimate goal of the Center is to eliminate the transmission and stigma of hepatitis B, and reduce deaths from liver cancer and liver disease caused by chronic hepatitis B.
Learn more on their website
Dan Azagury, MD
Dr. Azagury’s research interests align with his clinical and teaching endeavors. He has two main areas of interest: medical innovation and novel technologies, and foregut and bariatric procedures and outcomes. His outcomes research focuses on the effects of bariatric surgery on the all aspects of patient’s health as well as long-term outcomes. His other area of interest revolves around innovation: how to develop novel and relevant medical devices, how to evaluate their impact and cost/benefit for patients, and how to implement novel technologies to solve current unmet needs. His research projects often include multidisciplinary collaborations including with gastroenterologists, cardiologists, neurosurgeons, engineers and computer scientists.
CAP Profile
Aaron J. Dawes, MD, PhD
Dr. Dawes’s research focuses on understanding and improving care for vulnerable populations with cancer. His current work is split between quantitative health policy analysis and qualitative/mixed-methods community-engaged research. In his policy work, he is currently studying 1) the impact of Medicaid managed care on high-risk populations, 2) measures of network adequacy and the impact of network adequacy regulation on access to specialty cancer care, and 3) how the safety-net workforce has responded to capitation. In his community-engaged research, he is exploring 1) barriers and facilitators to the receipt of recommended cancer care in the Latino community and 2) the use of community health workers ( promotoras ) as navigators for patients with newly diagnosed colorectal cancer. His long-term goals involve forming partnerships with local communities and government officials to help develop and implement data-driven policy interventions to improve access and quality of cancer care.
Dan Delitto, MD, PhD
Dr. Delitto’s research focuses on novel immunotherapeutic approaches to fibrotic tumors, particularly pancreatic cancer. His goals are to change the pattern of inflammation produced by fibroblasts to create an environment permissible to antitumor immune responses. He is also working in collaboration with investigators at Johns Hopkins on an implantable hydrogel vaccine applied to threatened surgical margins, with encouraging preclinical data suggesting margin sterilization is attainable. Learn more on the Delitto Lab website .
Frederick M. Dirbas, MD
Dr. Dirbas's research focuses on accelerated, partial breast irradiation, and within that even more specifically intra-operative radiotherapy for breast cancer (IORT). Currently, he is also collaborating with Michael Clarke, MD, of the Stanford Stem Cell Institute investigating the role of breast cancer stem cells in the radiobiology of breast cancer, specifically: tumor quiescence, resistance to therapy, and late recurrence.
Monica Dua, MD
Dr. Dua participates in the Benign Pancreas Program at Stanford and her outcomes research includes both benign and malignant aspects of GI/HPB surgery with a focus on the management of severe pancreatitis as well as surgical strategies for the treatment of necrotizing pancreatitis. Other research interests include the application of minimally invasive approaches to the surgical management of HPB diseases including laparoscopic techniques in liver surgery and the use of laparoscopic and robotic platforms in pancreatic surgery. She currently has an ongoing clinical trial looking at the myoelectric activity of the stomach following pancreaticoduodenectomy as a function of predicting which patients are at higher risk of developing delayed gastric emptying or postoperative ileus. This study is being performed concurrently with the introduction of the division’s enhanced recovery after surgery perioperative care pathways to facilitate improved patient outcomes in those undergoing pancreatic resections.
Dr. Dua was also awarded funding this year as a Co-PI on a Stanford Cancer Center proposal to implement the collection of patient-reported outcomes for GI Oncology (specifically HPB) patients. The specific aims of this study are to create disease-specific quality of life questionnaires and build them into the electronic medical system; to operationalize their distribution and collection in the outpatient clinics and MyHealth; and to build the capability to run individual and aggregate reports on patient-reported outcomes. This infrastructure for collecting disease-specific patient-reported outcomes will not only help clinicians understand the subjective patient experience but also improve the process of treatment decision-making, ultimately improving the quality of care.
Dan Eisenberg, MD
Dr. Eisenberg’s research interest is in obesity and metabolic & bariatric surgery (MBS) in special populations. Specifically, he is studying surgical outcomes in Veterans with severe obesity who represent a high-risk cohort of surgery. Recent funded research included evaluating the quality of health screening in Veterans with obesity. In addition, Dr. Eisenberg received a Merit Award from the Veterans Affairs Health Services Research & Development to study the quality of obesity screening and care in Veterans with spinal cord injury, with a goal to identify gaps in assessment and management in this special population.
Joe Forrester, MD
Dr. Forrester’s research portfolio is broad and includes priority areas of i) chest wall injury including operative and non-operative management of rib and sternal fractures; ii) novel therapies to manage enterocutaneous and enteroatmospheric fistulae, and clinical and in silico investigations designed to better understand interactions between the microbiological world and the surgical patient. Dr. Forrester also writes clinical practice guidelines for national organizations to help standardize and improve the care of surgical patients.
Dr. Forrester has received continuous extramural funding since becoming faculty and he has led trainees in receiving institutional- and national-level research grants. His mentorship philosophy is to encourage mentees to identify projects they are passionate about and then provide structured, step-wise guidance on their path to research independence.
Dr. Forrester is open to working and collaborating with undergraduates, medical students, post-graduate students, and fellow faculty. Please email [email protected] with any questions or interest.
Brooke Gurland, MD, FACS, FASCRS
Pelvic floor dysfunction affects 20% of women and <10 % of men over their lifespan. Treating pelvic floor dysfunction crosses a series of disciplines in urology, gynecology, gastroenterology, and colorectal surgery. These clinical issues — critical to Women’s Health — range from urinary and fecal dysfunction, pelvic organ prolapse, and evacuatory dysfunction to pelvic floor spasm and chronic pain.
At the Multidisciplinary Pelvic Health Center at Stanford, we have a robust prolapse registry that addresses patient profiles, risk factors for prolapse recurrence, pelvic floor imaging, surgical decision making and complications. We have currently received funding to perform a multicenter study that evaluates the cost effectiveness of combined rectal and vaginal surgery.
Mary Hawn, MD, MPH
Dr. Hawn’s area of research is health services researcher focusing on surgical quality measurement and policy. She has a background and training in epidemiology coupled with her leadership roles in surgical quality measurement. Her expertise and extensive experience in evaluation of surgical quality process and outcome linkage has impacted national policy and changed guidelines. She has performed a comprehensive evaluation of the Surgical Care Improvement Project (SCIP) implementation using national VA data. Defining robust metrics of surgical quality that are actionable and can lead to sustained improvement in our field are of utmost importance.
She also has experience with risk prediction modeling for surgical patients. During the Decision Support for Safer Surgery study she and her team developed models of real-time risk prediction for major complications and prospectively validated our models in patients and with expert surgeons. They were able to discern where computational risk prediction has added value and where it falls short. They currently have several ongoing national studies investigating readmissions following major surgical procedures to identify opportunities for improving care and reducing costs as well as de-implementing low value care.
Mardi Karin, MD
Dr. Mardi R. Karin’s primary interest is in optimizing clinical outcomes for nipple sparing mastectomy and breast reconstruction. Given the recent advances in breast MRI imaging, that now allows for 3D MRI image reconstruction and detailed viewing of the blood supply to the nipple area, this additional information can be used as a guide to the blood flow patterns to the nipple. Dr. Karin uses 3D Breast MRI images to identify blood flow patterns to the nipple, to develop surgical techniques to preserve blood flow to the nipple for optimal results with nipple sparing mastectomy. By prospectively tracking clinical outcomes, it appears that this improved ability to preserve blood flow to the nipple results in lower rates of nipple necrosis and mastectomy skin necrosis that can occur as a result of poor perfusion, and thus improved clinical outcomes. Clinical outcomes are evaluated and tracked by Dr. Karin in collaboration with the Plastic and Reconstructive surgeon, Dr. Arash Momeni and others. It is hoped that this will translate into shorter healing time for patients, and also ultimately more optimal cosmetic outcome with nipple-sparing mastectomy and breast reconstruction.
Electron Kebebew, MD
Dr. Kebebew’s clinical and translational research is focused on three main scientific goals: 1) to develop effective therapies for fatal, rare and neglected endocrine cancers by identifying driver genomic/genetic events that govern cancer initiation/progression; 2) to identify new methods, strategies and technologies for improving the diagnosis of endocrine neoplasms and the prognostication of endocrine cancers; and 3) to develop methods for precision treatment of endocrine tumors utilizing genomic/genetic information and advanced imaging modalities.
Visit the Endocrine Oncology Lab website
Cindy Kin, MD
Dr. Cindy Kin is a colorectal surgeon whose research interests include treatments and outcomes of inflammatory bowel disease, medical decision-making in surgical patients, and implementation and outcomes of enhanced recovery pathways. She uses both quantitative and qualitative research methods to address these questions. Current projects include: biologic use and surgical complications among patients with inflammatory bowel disease, the use of opioids among patients undergoing surgical procedures and prescribing practices of surgeons, the effect of a multimodal prehabilitation program on patient experience and outcomes, and medical decision-making among patients with inflammatory bowel disease.
Lisa Knowlton, MD, MPH
Dr. Knowlton is a trauma and critical care surgeon and health services researcher who is currently an Assistant Professor within the Department of Trauma Surgery and Surgical Critical Care at Stanford University Medical Center. Using mixed methodologies and advanced geospatial mapping techniques, she has conducted evaluations of access to safe surgery in numerous low- and middle-income countries. This research has resulted in collaborations with the World Health Organization, non-profits, government officials and Ministries of Health. In addition to her global health expertise, she has most recently focused on better understanding the complex interplay between local access to healthcare and patient outcomes. This is particularly relevant to trauma patients, where significant disparities exist based upon socioeconomic and insurance status, and the financial burden of injury can be devastating for underinsured trauma patients and the hospitals in which they are treated. She has been awarded the 17th C. James Carrico Faculty Research Fellowship by the American College of Surgeons to better understand the link between socioeconomic status, insurance coverage and quality of patient outcomes for trauma patients receiving care within U.S hospitals.
Future goals of her research curriculum include developing novel reimbursement initiatives for quality trauma care, providing economically sustainable strategies for ensuring best outcomes among trauma patients and long-term viability of our essential trauma systems.
James R. Korndorffer, Jr. MD, MHPE, FACS
Dr Korndorffer’s research interest and focus is on education and assessment of medical learners—including undergraduate medical education learners, graduate medical education learners and the practicing physician lifelong learners. He has been involved in developing and evaluating novel teaching strategies, as well as unique assessment and evaluation methods.
A large body of his research focuses on the use of simulation for learning and assessment. He was an early adopter of the use of simulation for surgical training and has been actively involved in this research since 2003. He performed some of the early work using proficiency-based training instead of time base training for skill acquisition. This has now become the norm—whether called proficiency-based training or mastery learning.
He has continued this programmatic research with additional emphasis on simulation for assessment. It is this focus on assessment that has been recognized nationally. His additional area of interest is in patient safety and quality improvement through teamwork in the hospital environment. Combining these two areas he is investigating the role simulation education has in patient care quality and healthcare system safety.
Dana T. Lin, MD
Dr. Lin’s primary research focus is in surgical education, specifically around curriculum design, and cognitive and technical skills acquisition and assessment. Her projects leverage technological innovation such as gamification, mobile applications, and video-based learning to enhance surgical training. Her research team created ENTRUST, a serious game-based virtual patient simulation platform to teach and assess medical and surgical decision-making. The platform has been employed among United States general surgery residency training programs to assess clinical decision-making for Entrustable Professional Activities (EPAs). ENTRUST has also been utilized globally with principal collaborators from the College of Surgeons of East, Central, and Southern Africa (COSECSA), University of Global Health Equity (UGHE) in Rwanda, Alzaiem Alazhari University in Sudan, as well as Intuitive Surgical’s global Surgical Education Learners Forum.
Arden M. Morris, MD, MPH
Implementation of the Synoptic Operative Report for Rectal Cancer May 2018
Arden M. Morris, MD, MPH is Professor of Surgery and Vice Chair for Clinical Research in the Department of Surgery. She recently served on the National Quality Forum Consensus Standards and Approval Committee and was a Visiting Scholar at the Russell Sage Foundation. As a practicing surgeon and health services researcher, she uses quantitative and qualitative methods to focus on quality, patient centered care, and disparities in care. Dr. Morris is completing analyses for a collaborative multicenter mixed methods study to understand patient and provider influences on decision making and the quality of colorectal cancer care. Her results have provided critical information on the importance of doctor-patient communication, patient values, and socioeconomic considerations in shaping treatment decisions. She next intends to study the implementation of patient-centered policies in ways that support patient-provider relationships, facilitate coordination of care, and explicitly engage patients in their care.
Dr. Morris was recently recruited by Stanford University to develop and lead the Stanford-Surgery Policy Improvement Research and Education (S-SPIRE) Center . With goals to improve the value of healthcare through research that informs policy and implementation, to develop innovative mixed methodologies, and to create a community of surgical health services researchers at Stanford, S-SPIRE Center has already assembled an interdisciplinary team that includes clinical and research faculty with expertise in implementation science, health economics, bioinformatics, and quantitative, qualitative, and mixed methodologies.
Aussama Nassar, MD, MSc, FACS, FRCSC, CHSE
Dr. Nassar, is a clinician and simulation educator with a Master’s degree in Health Sciences Education. His educational research focuses on creating educational assessment tools, the use of simulation based medical education in team training, inter-professional team education and collaboration for trauma and the operating room. Dr. Nassar is currently spearheading a team of researchers in developing a conceptual framework for inpatient focused communication skills curriculum for surgical residents. Furthermore, he is leading a study looking at the utility of in-situ virtual reality simulation for trauma team inter-professional team education and debriefing.
In addition to his educational focus, Dr. Nassar has special research expertise in physician wellness and particularly burnout among academic clinicians.
Jeff Norton, MD
Dunphy's Puzzle Revisited: Is it time to consider antitumor immunity in cancer research. Sept. 2018
Gene Directed Surgery Dec. 2017
Tumors are composed of tumor cells and stroma. My research, in collaboration with Dr. Longaker in the Division of Plastic & Reconstructive Surgery, is investigating the tumor stroma to determine if it can be used to affect tumor growth and recurrence. Our initial work has focused on fibroblasts because they are the most common cellular component of the tumor stroma, but in the future, we will also investigate the immune cellular component and signaling molecules like cytokines and growth factors. My prior research focused on the role of cytokines and growth factors in wounds and tumors so I intend to further investigate these factors in our current models with the eventual goal of affecting tumor growth, progression and metastases.
Carla Pugh, MD, PhD
Carla Pugh, MD, PhD is the Thomas Krummel Professor of Surgery at Stanford Medicine and Director of the Technology Enabled Clinical Improvement (T.E.C.I.) Center. Her clinical area of expertise is Acute Care Surgery and her research involves the use of simulation, advanced engineering technologies, and artificial intelligence to develop new approaches for assessing and defining mastery in clinical procedural skills. Dr. Pugh is considered to be a leading, international expert on the use of sensors and motion tracking technologies for performance measurement.
See Technology Enabled Clinical Improvement Center
George Poultsides, MD
The main focus of Dr. Poultsides’ research team lies on clinical outcomes analysis following multidisciplinary treatment of hepatic, pancreatic and gastrointestinal malignancies. He has led several nationwide, multi-institutional clinical research collaborations across several academic medical centers in the US on liver, pancreatic, adrenal and gastric cancer. Within Stanford, Dr. Poultsides has developed a novel interdisciplinary research program assessing the completeness of surgical resection for pancreatic cancer. He has served as the principal investigator in two, first in human, prospective clinical trials evaluating the role of mass spectrometric and intraoperative fluorescent imaging during surgery for pancreatic cancer. These research efforts were funded through the 2012 Stanford Hospital Cancer Innovation Fund award and the 2016 Stanford Cancer Institute translational research award.
View a complete list of the group's scholarly contributions
S-SPIRE Center
S-SPIRE is a community of surgeon-scientists dedicated to improving the value of healthcare through research that informs policy and implementation; promoting a surgical health services research community through mentorship and collaboration; and developing innovative mixed methodologies.
Our interdisciplinary team includes clinical and research faculty with expertise in implementation science, health economics, bioinformatics, and quantitative, qualitative, and mixed methodologies. For more information about opportunities for research collaboration, educational programs, and a summer healthcare career pipeline program for teens from low-income high schools, please visit our website.
Alex Sox-Harris, PhD
Dr. Sox-Harris is a health services researcher, applied statistician, and implementation scientist with several programs of research: quality measurement, predictive modeling, and de-implementation of low value treatments and practices. His quality measurement research across diverse clinical areas has informed measurement science methodology and measure selection by federal agencies and healthcare systems. His current focus is on the development and validation of quality measures for hand surgery, as well as testing strategies to use quality data to drive target behaviors, without causing unintended consequences. His predictive modeling research has focused on musculoskeletal disorders for which surgery is a major treatment option. He recently completed a 4-year VA-funded study that developed the best-in-class prediction models for short-term complications and 1-year improvements in pain and functioning for patients receiving elective total knee and hip replacement.
Dr. Sox-Harris is currently leads a VA-funded study to describe, understand, and reduce low value preoperative testing for patients undergoing low risk surgeries. Future plans include examining a more comprehensive group of low value surgical practices, and developing and testing organizational interventions to improve practice and clinical outcomes. Dr. Sox-Harris also mentors early career surgeon-scientists in the art and craft of building health services research careers.
David A. Spain, MD
Dr. Spain is an investigator in the field of Acute Care Surgery (Trauma, Emergency and Critical Care Surgery). Along with Eve Carlson, PhD, they were recently PI on an R-01 grant from the National Institute on Minority Health and Health Disparities (NIMHHD) on the “Development of a Risk Factor Screen for Mental Health Problems after Sudden Illness or Injury.”
Along with Dr. Knowlton, Dr. Spain is also the site co-PI on a large multi-institutional trial funded by the DOD - Defense Medical Research and Development Program on “The Pathogenesis of Post-Traumatic Pulmonary Embolism: A Prospective Multi-Center Investigation by the CLOTT Study Group.”
Kristan Staudenmayer, MD, MS
Dr. Staudenmayer’s research has focused using secondary data to generate knowledge around trauma and emergency general surgery systems of care. She has been an active PI funded by the NIH (NIA K08) and the Clinical and Translational Science Award Program. Her research focus has historically been on vulnerable populations, especially those who are financially disadvantaged as well as older adults. These populations are particularly affected by emergent surgical conditions such as trauma or emergency general surgery diagnoses. She has also worked to improve systems of care for these populations. Her body of work on trauma systems aims to evaluate the economically viability of trauma systems, which is necessary to ensure high-quality trauma care can be delivered in the U.S. She also has experience in informatics.
Her most recent work is exploring the development of systems for management of health-related data in electronic health records and mechanisms to automate data utilization for downstream purposes such as point-of-care tools funded through Stanford and the American College of Surgeons. Dr. Staudenmayer has recently submitted a grant to the NIH in conjunction with the ACS with the goal of automating electronic registry creation to facilitate research and quality efforts.
Furthermore, Dr. Staudenmayer holds leadership roles in national academic societies including the American College of Surgeons and the American Association for the Surgery of Trauma. This allows her to shape health services research topics in national trauma and emergency general surgery systems at a national level.
Technology Enabled Clinical Improvement Center
The Technology Enabled Clinical Improvement (T.E.C.I.) Center is a multidisciplinary team of researchers dedicated to the design and implementation of advanced engineering technologies that facilitate data acquisition relating to clinical performance.
The T.E.C.I. team has had great success in quantifying physicians’ clinical experiences using sensor, video, and motion tracking technologies. This work has resulted in an information rich database that enables empirical evaluation of clinical excellence and medical decision making.
By leveraging highly specific and objective clinical performance metrics, the T.E.C.I. Center is harnessing the unique opportunity to support peer to peer data sharing and clinical collaborations that can transform the clinical workflow and ultimately benefit healthcare providers.
The T.E.C.I. Center aims to transform human health and welfare through advances in data science and personalized, technology-based performance metrics for healthcare providers.
Learn more on the website
Jacqueline Tsai, MD, FACS
Dr. Tsai’s research interest and focus are improving technologies for breast cancer localization. She is currently collaborating with radiology and engineering on augmented reality techniques for intraoperative tumor localization. Previous work has demonstrated improved localization with incorporating tumor sonification with localization devices. These new technologies may enhance tumor visualization and eventually lead to more accurate lumpectomy surgeries with fewer positive margins.
Additionally, Dr. Tsai has collaborated on several projects evaluating the importance of lymph node localization following neoadjuvant treatment, these include evaluation of methods of localization and clinical outcomes utilizing lymph node ratios.
Brendan C. Visser, MD
Dr. Visser is the Section Chief of HPB Surgery and the Medical Director of the GI Cancer Care Program at the Stanford Cancer Center. Dr. Visser’s research projects reflect the breadth of his clinical interests and activities. He currently has an active research collaboration with the Health Service Research team at S-Spire investigating “fragmentation” of care for gastrointestinal cancers (the receipt of care by a single patient at multiple centers and its impact on cancer outcomes). Working with the Loh Lab in Developmental Biology, Dr. Visser and Dr. Loh are investigating the recently discovered hormone GDF15, which is implicated in the malaise and anorexia associated with cancer and surgery—a troubling problem that affects many patients and can negatively impact their cancer journey. This is a multi-pronged project investigating GDF15 receptors in hind-brain neurons, the GDF15 response and and effects in mouse models of cancer surgery, and GDF15 levels in surgical patients. He the principal investigator in an active investigator-initiated clinical trial looking at peri-operative PRRT (peptide receptor radiotherapy) in adjunct with cytoreductive surgery for metastatic well-differentiated gastrointestinal (GI) neuroendocrine (NET) tumors. In addition to the analysis of clinical outcomes, this study includes the correlative science looking at the effects of the PRRT therapy on the tumors themselves. Dr. Visser is a key collaborator to the Dhanasekaran Lab, investigating genomic aspects of liver cancer in the search for novel biomarkers and therapeutics. Finally, as a busy clinical surgeon, Dr. Visser works with surgical trainees on outcomes projects to retrospectively analyze technical aspects of HPB surgery, strategies in the multidisciplinary management of hepatobiliary and pancreatic cancers, and the management of acute pancreatitis.
Todd Wagner, PhD
Dr. Todd Wagner studies health information, efficiency and value, and health care access. He is particularly interested in developing learning health care systems that provide high value care. He has worked for 20 years in a health care delivery system where economics and clinical care intersect with high-cost or intensive services, such as surgery or critical care.
Dr. Wagner’s work typically includes the analysis of large administrative datasets within the Stanford-Surgery Policy Improvement Research and Education (S-SPIRE) Center . He has a joint appointment with the Palo Alto VA where he directs of the Health Economics Resource Center and is the Associate Director for the Center for Innovation to Implementation. He also co-directs the Big Data Fellowship, which is supported by VA and NCI.
Dr. Wagner is finishing a study on specialty care access and the role of telemedicine in the VA. Current projects include a study estimating the causal effect of going to 12-step programs for drug abuse and the long-term follow-up from two cardiac surgery clinical trials.
Irene Wapnir, MD
Dr. Wapnir has longstanding interests in advancing the treatment of breast cancer through clinical trials and innovative approaches to surgery. She is currently accepting patients for a study testing the effectiveness of neoadjuvant partial breast radiation in the treatment of ductal carcinoma in situ (DCIS). This is a unique prospective randomized trial offered only at Stanford Cancer Institute. Click here to learn more about the DCIS clinical trial.
Additionally, Dr. Wapnir is the institutional lead for numerous other multicenter trials. Her prospective and retrospective studies using fluorescent guided skin angiography and devascularization of the nipple-areolar complex/two-staged nipple-sparing mastectomies have demonstrated superior outcomes. One of the most exciting innovations led by Dr. Wapnir and Dr. Dung Nguyen from Plastic Surgery, has been the development of a new type of post-mastectomy free-flap breast reconstruction using omentum. She is currently researching the long-term volume and symmetry outcomes of these patients.
Thomas G. Weiser, MD, MPH
Lifebox Global
His research is focused on evaluating the role surgical care plays in the delivery of health services in resource poor settings, in particular low and middle income countries. He is interested in barriers to access and provision of surgical care, the quality of surgical services, and outcomes research as well as the science of implementation, how improvements can be made, and how to strengthen compliance with best practices and change behaviors for the better. He also has an interest in domestic policy as it relates to trauma outcomes, trauma systems, insurance coverage and costs of care, and firearm violence.
His current projects focus on the quality of surgical care and strategies for improving the safety and reliability of surgical delivery in resource poor settings. He is the Consulting Medical Officer for Lifebox, a nonprofit focused on improving surgical and anesthetic safety worldwide. Lifebox delivers programs throughout the world in combination with local partners including individual professionals, professional societies, hospitals, other NGOs, and ministries of health. Lifebox works with hospitals in Ethiopia, Liberia, Madagasgar, India, Honduras, and Nicaragua, amongst others, to improve care and evaluate the impact of our work. A few programs of particular impact are the distribution of low cost devices to improve the safety of care (including pulse oximeters for the routine monitoring of patients undergoing anesthesia and a new surgical headlight program) and Clean Cut, a surgical infection prevention and control program now being introduced in several countries.
Dr. Weiser has been involved in surgical program assessment projects in numerous countries. From 2006-2009, he was part of the World Health Organization’s Safe Surgery Saves Lives program where he quantified the global volume of surgery and created, implemented, evaluated, and promoted the WHO Surgical Safety Checklist. He has worked with the WHO and the World Bank and is currently the recipient of a Gates Grand Challenge grant to improve the safety of cesarean section in Ethiopia.
Visit his website
Sherry M Wren MD, FACS, FCS(ECSA)
Dr. Wren’s research program has international and domestic components. Internationally, she investigates access or barriers to care in humanitarian conflict zones and low and middle-income countries. In the humanitarian context, she is actively working to redesign surgical care delivery in the humanitarian response to modern conflicts. This work includes surgical disease epidemiology, logistic and response design, international humanitarian law, and policy implications of humanitarian responses, as well as developing tools to assess the quality of surgical care in these complex settings. In the non - humanitarian context in low and middle-income countries, Dr. Wren is using a gender lens to examine barriers to women obtaining surgical care and identifying opportunities to address the disparities and under-representation of women as surgical patients in hospitals. Within the US, Dr. Wren is interested in outcomes-based research, primarily within the VA system, to examine perioperative care, robotic surgery, and risk assessment in surgical patients.
Faculty Research Initiatives
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Surg J (N Y)
- v.8(4); 2022 Oct

General Surgery: Requirements, Rationale, and Robust Results
1 Department of Paediatrics, Military Hospital Secunderabad, Secunderabad, Telangana, India
Ashok Puranik
2 Trauma Care and Acute Care Surgery, Monash University Australia, Melbourne, Australia
3 Executive Director, All India Institute of Medical Sciences (AIIMS) Guwahati, Assam, India
Safe, timely, and affordable surgical care is desirable worldwide, but is largely an unmet need. Surgical care is recognized as an important component of public health. Vision for sustainable surgical development is desirable, and general surgeons can contribute substantially toward this mission.
In the absence of surgical care, case-fatality rates are high for common and easily treatable conditions. These include congenital anomalies, hernia, fractures, appendicitis, etc. Solution is surgical care. Results of surgery on time are rewarding.
General surgeons, as per the Medical Council of India, are required to (1) recognize the health needs of the community and carry out professional obligations, (2) be competent, and (3) be aware of the contemporary advances and developments in the discipline concerned. All this ensures that the general surgeon should be able to treat almost all surgical conditions effectively.
With timely, cautious, careful, and tactful surgeries, general surgeons should be able to deliver robust results both electively and in emergency. All this in the true spirit of “Vayam Sevaamahe – We are for service” the motto of the Association of Surgeons of India. General surgeons should boost the best what was termed “ Professional patriotism ” in the historic Flexner report.
Surgical care is recognized as an important component of public health. 1 Five billion people worldwide do not have access to safe, timely, and affordable surgical and anesthesia care. This results in over 18 million deaths each year and one-third of the global burden of disease. 2
Against this background, our article's aim is to (1) analyze general surgery (GS) requirements, (2) build upon the rationale for the role general surgeons should be playing, and (3) catalyze the results which general surgeons can produce.
Strategies for sustainable surgical development are desirable and should aim for quality dividends quantitatively. Access to the full spectrum of health care, including surgical care by all has to be achieved. Surgically treatable conditions account for a significant proportion of the total global burden of disease, and surveys of need have shown that it is largely unmet. 3 4 Recently, it has been reported that the world's population without access to surgical care is significantly greater than previously reported. The modeling study estimates that at least 4.8 billion people do not have access to surgical care. 5 General surgeons can play an important role. Personal aptitude for surgery and professionally armed with skills, general surgeons can deliver results.
Professional approach to health for all and advancing modern surgery, demands wide expertise by all against the present trend of limited expertise by only a few for a limited field—the so-called sub(super)-specialization. Majority of the surgical conditions can be dealt by general surgeons and they are trained in it. Holistic healing requires leadership, understanding of human as a whole, and not just organ- or system-specific superspecialist surgeons.
The Requirements
Lancet Commission on Global Surgery estimated need of 5,000 surgeries per year per 100,000 population. 6 In India, it has been estimated that 3,646 surgeries are required per 100,000 Indian population per year. 7 Of these, 26% would be general surgical procedures, 20% would be obstetrics and gynecological surgeries, and 13% would be ophthalmological surgeries.
In the absence of surgical care, case-fatality rates are high for common and easily treatable conditions including congenital anomalies, hernia, fractures, appendicitis, etc. These conditions are ubiquitous. Solution is surgical care. Results of surgery on time are rewarding. 8
India's doctor-population ratio of 1:854 is better than the World Health Organization (WHO) standard of 1:1,000. 9 Estimates of the stock of surgeons in India range between 1.5 and 6.8 per 100,000 population. India continues to experience shortages of health workers despite impressive increases in production capacity in recent years. The production capacity of surgical specialists in India has experienced an upward trend in recent years, and in 2015 it was estimated to be 2,131. 10 The number of super- or subspecialist surgeons are abysmally low. General surgeons have to and can play an important role.
With universal coverage of essential surgery in low-income and middle-income countries, 1.5 million deaths per year could be averted, representing 6.5% of all avertable deaths in these countries. 11 Morbidity figures can be much more. It has been suggested that as an interim measure, multiskill training of general doctors to reduce the deficit of surgical specialists, particularly at community health centers, should be expanded. 10
Worldwide statistics reveal other aspects as well. Available statistics show that over 44% of WHO Member States report to have less than 1 physician per 1,000 population. Health workers are distributed unevenly across the globe. Countries with the lowest relative need have the highest numbers of health workers, while those with the greatest burden of disease must make do with a much smaller health workforce. 12
It has been commented that essential surgery provisioning in rural and remote areas can be only partly met both in developed and in low- and middle-income countries. It may take years to solve the problem of unmet needs. 13 General surgeons should play an increasingly important role in reaching and serving all.
The scenario of surgeons in the Indian Armed Forces is peculiar. The needs are both peace-time and war-time. In addition, surgeons of the Indian Armed Forces play an important role in relief operations. They also play important role by way of surgical camps like those of Op Sadbhavana, in remote and underserved locations.
The Rationale
The World Federation for Medical Education Global Standards 2015 for Postgraduate Medical Education stipulates to base the mission on consideration of the health needs of the community or society. 14 Similarly, the General Medical Council, U.K., specifies that postgraduate training should be responsive to adapt to current and emerging patient and population needs. 15 All this, against the backdrop of requirements, points to an increasingly important role the general surgeons should be playing in serving the surgical needs of populations.
The goal of postgraduate medical education shall be to produce competent specialists. General surgeons awarded MS degrees are expected to have the following competency as per the Medical Council of India (now the National Medical Commission) 16 :
First, recognize the health needs of the community, and carry out professional obligations ethically and in keeping with the objectives of the national health policy. Important implication is to meet all the surgical needs of the community.
Second, mastered most of the competencies, pertaining to the speciality, that are required to be practiced at the secondary and the tertiary levels of the health care delivery system. All the needs of communities, states, and nations can be met for by general surgeons in these levels of health care.
Third, be aware of the contemporary advances and developments in the discipline concerned. Surgeons have the enthusiasm, and with sustained efforts for ongoing training the general surgeon should be able to treat almost all surgical conditions effectively.
A meeting of experts for workable solutions for GS workforce shortfalls recommended to enhance the number of GS trainees and the breadth of training. It also recommended that minimally invasive surgery should largely return to GS. 17 Feasibility of minimally invasive surgical procedures in the outpatient setting is a further boost. 18 Similarly, an Indian peer review of teaching, training, and evaluation in GS has pointed out that it should be broad based and skills should be open and endoscopic. 19 General surgeons need to learn, practice, and master the latest trends. All this will lead to professional progress, self-satisfaction, and satisfaction of the masses.
Surgeons have long been considered leaders in adapting and improving their practice. 20 Latest evidence is useful and needs to be implemented. Engagement in a growing number of free-to-use “Web portals” (e.g., General Surgery—Medscape, available at http://www.medscape.com/generalsurgery/ ) and medical media communication (e.g., General Surgery News, available at http://www.generalsurgerynews.com/ ) is useful in assimilating the newest evidence.
Formal online courses, webinars, and remote telementoring all provide examples of surgical leadership. 21 All these should be used by general surgeons for progressive improvements.
Professionalization of modern surgery demands wide expertise by all against the present trend of limited expertise by only a few for a limited field—the so-called subspecialization.
Professionalism has been defined as “a set of values, behaviors, and relationships that underpins the trust the public has in doctors.” 22 Competence is an important attribute of professionalism, in relation to surgical practice. 23 Thus, a general surgeon should be competent in dealing with almost all conditions. Subspecialization expertise is required for only few conditions. Further, tactful supportive follow-up strategies can ensure healthy well-being after complex surgeries. 24 General surgeons can play an important role in this respect as well.
General surgeons need to be energized for excellence: It requires sustained energy for excellence, to achieve the targets, and to stay high on the results. With all this we should be able to meet the unmet needs. 25
Robust Results
Improvements in antisepsis, advanced anesthetic techniques, and sophisticated surgical skills have led to improvement in outcomes for surgical patients. Surgery can be elective or performed in emergency. Identifying predictors of mortality and surgical complications has led to outcome improvements for a variety of surgical conditions. 26 Recent studies have shown that emergency GS patients are at uniquely higher risk for medical errors and complications following surgery, with emergency GS patients up to eight times more likely to die compared to patients undergoing the same procedure electively. The excess morbidity and mortality of emergency GS are not fully explained by preoperative risk factors, making emergency GS an excellent target for quality improvement projects. 27 28 All this points to need for timely and careful surgical intervention.
An illustrative example of need for timely surgical intervention is a common condition—inguinal hernia. A hernia not operated is a cause of morbidity, and complications of hernia are a potential cause of mortality. Risks of surgery are substantially less and results rewarding. Approximately 50% of inguinal hernias manifest clinically in the first year of life, most in the first 6 months. The incidence of complications associated with elective hernia repair (intestinal injury, testicular atrophy, recurrent hernia, wound infection) are low (≈1%), but rise to as high as 18 to 20% when repair is performed at the time of incarceration. Elective inguinal hernia repair can be safely performed in an outpatient setting with an expectation for full recovery within 48 hours. 29 All these point toward need of delivery by general surgeons.
Adverse events in surgery are an important problem globally. Many are preventable. The WHO Surgical Safety Checklist has been shown to reduce surgical complications and improve communication and teamwork in the operating theatre. 30 31 Feasible measures, such as WHO's Surgical Safety Checklist, lead to improvements in safety and quality. The basic and essential objectives for safe surgery according to WHO are: Operate on the correct patient at the correct site; Use method known to prevent harm from anesthetic administration, while protecting the patient from pain; Recognize and effectively prepare for life-threatening loss of airway or respiratory function; Recognize and effectively prepare for risk of high blood loss; Avoid inducing any allergic or adverse drug reaction known to be a significant risk for the patient; Consistently use method known to minimize risk of surgical site infection; Prevent inadvertent retention of instruments or sponges in surgical wounds; Secure and accurately identify all surgical specimens; Effectively communicate and exchange critical patient information for the safe conduct of the operation; Establish routine surveillance of surgical capacity, volume, and results. 32
An important quality improvement initiative is clinical audit. The process involves comparing aspects of care (structure, process, and outcome) against explicit criteria and defined standards. General surgeons should analyze results and compare performance against agreed standards with regular audit. It also documents track of personal clinical results. Rigorous evaluation of even the most simple techniques and conditions should be done. It can help to keep a surgeon stimulated throughout a long career and ensure good outcomes for patients, with cost benefits to the provider and a benefit to society as a whole. 33
With timely, cautious, careful, and tactful surgeries general surgeons should be able to deliver robust results both electively and in emergency. More sophisticated surgical operations with better results are increasingly performed. General surgeons should also continue to increase their skills and sophistication.
Advancements in technology hold great promise for the advancement of patient care. Modern technology enriches (1) proper assessment, (2) pertinent management, including surgical intervention, (3) progress monitoring, including for adverse events, 34 (4) prevention of progress/worsening/complications, (5) professional standards achievement, improvement, and maintaining them, and (6) patient safety. 34 General surgeons should utilize these.
The practice of surgery is changing in significant ways, and for the good. Novel techniques often require an entirely novel skill set for surgeons. General surgeons should embrace and master new techniques throughout their careers.
The latest trend in training in the context of a larger curriculum of proficiency-based training in surgery is encouraging. It is the best way to achieve good training results. 35 Procedural skills training in a simulated environment, including virtual reality training, has been shown to transfer to the real-life clinical setting. Virtual surgical planning increases confidence and knowledge for surgery for better outcomes. 34 All this should be utilized for training many, for serving all.
“Vayam Sevaamahe – We are for service” is the motto of the Association of Surgeons of India. Surgical care and cure for all should not be a distant dream in India and worldwide, with dedication and devotion of all the general surgeons. General surgeons should strive for service improvement and innovations in delivery of services for the benefit of patient care. The field of surgery is an ever-evolving one. General surgeons should improvise ways for delivery of all advances for the benefit of all.
In the present context the historic Flexner report, 36 which reformed medical education in the United States, should continue to guide, reinforce, and rejuvenate the services by the general surgeons:
“ Professional patriotism amongst medical men: the regard for the honor of the profession and the sense of responsibility for its efficiency .”
Conflict of Interest None declared.

General Surgery Topics
- Bioterrorism and Disaster Medicine
- Breast Cancer
- Colorectal Cancer
- Inflammatory Bowel Disease
- Medical Malpractice and Legal Issues
- Methicillin-Resistant Staphylococcus aureus (MRSA)
- Minimally Invasive Gastrointestinal Surgery
- Pain Management
- Patient Safety
- Perioperative Nursing
- Vascular Disease
- Wound Management
All Medscape Topics
- Acute Coronary Syndromes (ACS)
- Acute Leukemia
- Adolescent Medicine
- Aesthetic Medicine
- Affordable Care Act (ACA)
- Alzheimer's Disease
- AMD and Retinal Disease
- Antibiotic Resistance
- Antiretroviral Therapy
- Anxiety Disorders
- Arrhythmia & EP
- Arthroplasty
- Atopic Dermatitis
- Atrial Fibrillation
- Bariatric Surgery
- Barrett's Esophagus
- Bioterrorism/Disaster Medicine
- Bipolar Disorder
- Bladder Cancer
- Bone and Mineral Disorders
- Benign Prostatic Hyperplasia (BPH)
- Brain Cancer
- C. difficile
- Cardiovascular Risk Reduction
- Cataract and Refractive Surgery
- Celiac Disease
- Child and Adolescent Psychiatry
- Chronic Kidney Disease
- Chronic Leukemia
- Cornea and External Disease
- Coronavirus (COVID-19)
- Cosmetic Dermatology
- Critical Care Nursing
- Crohn's Disease
- CVD Prevention
- Cystic Fibrosis
- Dental and Oral Health
- Diabetic Microvascular Complications
- Eating Disorders
- Electronic Health Records
- Emerging and Reemerging Infectious Diseases
- End-Stage Renal Disease
- Erectile Dysfunction
- Exercise and Sports Medicine
- Fibromyalgia
- Gallbladder and Biliary Disease
- Genomic Medicine
- Geriatrics-Palliative Care
- GI/Colorectal Cancer
- GI/Noncolorectal Cancer
- GU/Prostate Cancer
- Head and Neck Cancer
- Health Diversity
- Healthcare Reform & the ACA
- Heart Failure
- Hepatitis B
- Hepatitis C
- HIV Transmission & Prevention
- Hodgkin's Lymphoma
- Hospital Medicine
- HPV and Cervical Cancer
- Hypertension
- Hypogonadism
- IBS and Chronic Constipation
- Immunization
- Infertility
- Insulin Therapy
- Integrative Medicine
- Interventional Cardiology & Surgery
- Joint Disorders
- Kidney & Pancreas Transplant
- Lipids & Metabolic
- Liver & Intestine Transplant
- Lung Cancer
- Lyme Disease
- Mechanical Ventilation
- Medical Lifestyle
- Medical Practice Management
- Mental Health and Psychiatric Nursing
- Metastatic Breast Cancer
- Minimally Invasive Gastrointestinal Surgery (MIGS)
- Moderate to Severe Asthma
- Multiple Myeloma
- Multiple Sclerosis
- Neonatal Medicine
- Neurosurgery
- Non-Hodgkin's Lymphoma
- Novel Coronavirus
- Nurse Career and Education
- Nurse Practitioners
- OB/GYN and Women's Health Nursing
- Obesity and Weight Management
- Osteoarthritis
- Osteoporosis
- Otitis Media
- Otolaryngology
- Ovarian Cancer
- Palliative Care
- Pancreatitis
- Parenteral and Enteral Nutrition
- Parkinson's Disease
- Pediatric Dermatology
- Pediatrics/Neonatal Care Nursing
- Pediatric Ophthalmology
- Peptic Ulcer Disease
- Preclinical Studies
- Prostate Cancer
- Psoriatic Arthritis
- Pulmonary Arterial Hypertension
- Rare Diseases
- Reimbursement and Quality
- Renal Cell Carcinoma
- Reproductive Endocrinology
- Restless Legs Syndrome
- Rheumatoid Arthritis
- Schizophrenia
- Science and Technology
- Sjögren's Syndrome
- Skin Cancer
- Sleep Disorders
- Social Determinants of Health
- Spinal Disorders
- Stroke/Cerebrovascular Disease
- Substance Abuse and Addiction
- Systemic Lupus Erythematosus
- Thyroid Cancer
- Thyroid Disease
- Type 1 Diabetes
- Type 2 Diabetes
- Ulcerative Colitis
- Urinary Incontinence & OAB
- Women's Sexual Health
Featured Topics


- General Surgery
- Abdominal Abscess
- Abdominal Angina
- Abdominal Hernias
- Acute Abdomen and Pregnancy
- Acute Mesenteric Ischemia
- Bariatric Surgery
- Benign Gastric Tumors
- Benign Neoplasms of the Small Intestine
- Bile Duct Tumors
- Cholecystocutaneous Fistula
- Chyle Fistula
- COVID-19 Guidance for Surgeons
- Enhanced Recovery After Surgery (ERAS) in Emergency Abdominal Surgery
- Enterocutaneous Fistula
- Gallbladder Mucocele
- Gallbladder Tumors
- Gallbladder Volvulus (Torsion)
- Gastric Outlet Obstruction
- Gastric Volvulus
- Hepatic Cysts
- Hepatocellular Carcinoma (HCC)
- Inferior Vena Caval Thrombosis
- Inflammation of Vermiform Appendix
- Intestinal Fistula Surgery
- Intestinal Perforation
- Liver Abscess
- Meckel Diverticulum
- Mesenteric Tumors
- Neurogenic Bowel Dysfunction
- Omental Torsion
- Pancreatic Pseudoaneurysm
- Postcholecystectomy Syndrome
- Pressure Injuries (Pressure Ulcers) and Wound Care
- Radiation Enteritis and Proctitis
- Short-Bowel Syndrome
- Solid Omental Tumors
- Splenic Abscess
- Splenic Infarct
- Surgical Approach to Peritonitis and Abdominal Sepsis
- Surgical Treatment of Perforated Peptic Ulcer
- Temporary Abdominal Closure Techniques
- Anal Fissure
- Anorectal Abscess
- Fistula-in-Ano
- Gardner Syndrome
- Perianal Cysts
- Perianal Granuloma
- Pilonidal Cystectomy
- Pilonidal Disease
- Proctitis and Anusitis
- Proctitis and Proctocolitis Organism-Specific Therapy
- Pseudomembranous Colitis Surgery
- Rectal Prolapse
- Rectovaginal Fistula
- Sigmoid and Cecal Volvulus
- Benign Tumors of Major Salivary Glands
- Benign Tumors of Minor Salivary Glands
- Acute Frontal Sinusitis Surgery
- Bilobed Flaps
- Cerumen Impaction Removal
- Cheek Reconstruction Procedures
- Cleft Lip Nasal Deformity
- Craniofacial Distraction Osteogenesis
- Ear Reconstruction
- Forehead Flaps
- Forehead Reconstruction
- Mental Nerve Block
- Nasal Polyp Surgery
- Nitrous Oxide Administration
- Nonablative Resurfacing
- Pediatric Sinusitis Surgery
- Percutaneous Tracheotomy
- Peritonsillar Abscess
- Reconstructive Surgery for Cleft Palate
- Surgical Management of Chronic Aspiration
- Surgical Treatment of Acute Ethmoid Sinusitis
- Surgical Treatment of Acute Maxillary Sinusitis
- Surgical Treatment of Acute Sphenoid Sinusitis
- Surgical Treatment of Chronic Maxillary Sinusitis
- Transoral Parathyroidectomy
- Wrist Arthroscopy
- Axillary Dissection
- Lymphatic Leakage
- Phyllodes Tumor (Cystosarcoma Phyllodes)
- Abdominal Stab Wound Exploration
- Skin Grafting
- Wound Closure Technique
- Wound Healing and Repair
- Wound Infection
- Allergy & Immunology
- Anesthesiology
- Cancer Guides
- Cardiology Guidelines
- Clinical Procedures
- Critical Care
- Dermatology
- Emergency Medicine
- Endocrinology
- Gastroenterology
- Genomic Medicine
- Infectious Diseases
- Laboratory Medicine
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopedic Surgery
- Otolaryngology and Facial Plastic Surgery
- Pediatrics: Cardiac Disease and Critical Care Medicine
- Pediatrics: Developmental and Behavioral Articles
- Pediatrics: General Medicine
- Pediatrics: Genetics and Metabolic Disease
- Pediatrics: Surgery
- Perioperative Care
- Physical Medicine and Rehabilitation
- Plastic Surgery
- Pulmonology
- Rare Diseases
- Rheumatology
- Sports Medicine
- Thoracic Surgery
- Transplantation
- Vascular Surgery
- John Geibel, MD, MSc, DSc, AGAF

Jump to content
American College of Surgeons | Online Learning
Bookmark/search this post.

You are here
Ten hot topics in general surgery.

Accreditation
- Register/Take course
Session Description
In this popular session, the panelists review 10 of the hottest topics in general surgery selected from the ACS General Surgery Communities, recent surgery meetings, and the literature.
Course Outline
- Approaches to Femoral Hernia Benjamin K. Poulose, MD, MPH, FACS, Nashville, TN
- Pure Tissue Repair of Inguinal Hernia: Resurrection of a Lost Art John L. Tarpley, MD, FACS, FWACS, Nashville, TN
- Management of Symptomatic Gallstones in Pregnancy Rebecca C. Britt, MD, FACS, Norfolk, VA
- Laparoscopic Lavage vs. Hartmann Procedure for Perforated Diverticulitis Patricia L. Roberts, MD, FACS, FASCRS, Burlington, MA
- Oh, No! An Incorrect Count: Now What? Steven M. Steinberg, MD, FACS, Columbus, OH
- Hyperthyroidism: When Do I Recommend Surgery and What Is the Extent of Resection? Herbert Chen, MD, FACS, Birmingham, AL
- Current Management of Breast Abscess Wendy R. Greene, MD, FACS, FCCM, Atlanta, GA
- Incidental Liver Lesions: Treat or Observe? Cristina R. Ferrone, MD, FACS, Boston, MA
- Pneumatosis Intestinalis: Incidental or Catastrophic? Jose J. Diaz, MD, FACS, FCCM, Baltimore, MD
- Newer Approaches to Pancreatic Necrosis Steven J. Hughes, MD, FACS, Gainesville, FL
Target Audience
- Practicing surgeons
Learning Objectives
- Apply new knowledge and ideas to improve their surgical practice
- Adapt concepts and quality measures in support of research advancements
- Enhance the quality of patient care
- For questions about the course content, please contact [email protected].
- If you have any technical questions, contact [email protected].
- 1.50 AMA PRA Category 1 Credit™
- 1.50 Certificate of Completion
- 1.50 Self Assessment Credit
Disclosure Information
In accordance with the ACCME Accreditation Criteria, the American College of Surgeons must ensure that anyone in a position to control the content of the educational activity (planners and speakers/authors/discussants/moderators) has disclosed all relevant financial relationships with any commercial interest. For additional information, please visit the ACCME website: http://www.accme.org/requirements/accreditation-requirements-cme-providers/policies-and-definitions/financial-relationships-and-conflicts-interest
The ACCME also requires that ACS manage any reported conflict and eliminate the potential for bias during the educational activity. Any conflicts noted below have been managed to our satisfaction. The disclosure information is intended to identify any commercial relationships and allow learners to form their own judgments. However, if you perceive a bias during a activity, please report it on the evaluation.
(Download the full list of disclosures . )
Faculty and Disclosures
Benjamin K. Poulose, MD, MPH, FACS, Nashville, TN - Ariste Medical: Consulting Fee: Consultant Bard-Davol: Research Funds: Co-Investigator, Americas Hernia Society Quality Collaborative: Salary John L. Tarpley, MD, FACS, FWACS, Nashville, TN - No Disclosures Rebecca C. Britt, MD, FACS, Norfolk, VA - No Disclosures Patricia L. Roberts, MD, FACS, FASCRS, Burlington, MA - No Disclosures Steven M. Steinberg, MD, FACS, Columbus, OH - No Disclosures Herbert Chen, MD, FACS, Birmingham, AL - No Disclosures Wendy R. Greene, MD, FACS, FCCM, Atlanta, GA - No Disclosures Cristina R. Ferrone, MD, FACS, Boston, MA - No Disclosures Jose J. Diaz, MD, FACS, FCCM, Baltimore, MD - No Disclosures Steven J. Hughes, MD, FACS, Gainesville, FL - No Disclosures
Program Committee and Disclosures
CHAIR: Henri R. Ford, MD, MHA, FACS, FAAP, FRCSEng(Hon), Miami, FL - No Disclosures VICE-CHAIR: David T. Cooke, MD, FACS, Sacramento, CA - No Disclosures
David C. Borgstrom, MD, FACS, Morgantown, WV - No Disclosures Daniel L. Dent, MD, FACS, San Antonio, TX - No Disclosures Roger R. Dmochowski, MD, FACS, Nashville, TN - Allergen: Honoraria: Consultant Audra A. Duncan, MD, FACS, London, ON - No Disclosures Mariam F. Eskander, MD, Boston, MA - No Disclosures Paula Ferrada, MD, FACS, Richmond, VA - No Disclosures Neil H. Hyman, MD, FACS, Chicago, IL - No Disclosures Martin S. Karpeh, Jr., MD, FACS, New York, NY - No Disclosures Dennis H. Kraus, MD, FACS, New York, NY - No Disclosures Kenneth W. Sharp, MD, FACS, Nashville, TN - No Disclosures David A. Spain, MD, FACS, Stanford, CA - No Disclosures
Ex-Officios
Mary T. Hawn, MD, FACS, Stanford, CA - No Disclosures Daniel M. Herron, MD, FACS, FASBMS, New York, NY - No Disclosures
Consultants
Barbara Lee Bass, MD, FACS, FRCS(Hon), Houston, TX - No Disclosures Quan-Yang Duh, MD, FACS, San Francisco, CA - No Disclosures B. J. Hancock, MD, FACS, FRCSC, Winnipeg, MB - No Disclosures Ronald V. Maier, MD, FACS, FRCSEd(Hon), Seattle, WA - No Disclosures Valerie W. Rusch, MD, FACS, New York, NY - No Disclosures
Continuing Medical Education Credit Information
The American College of Surgeons is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
AMA PRA Category 1 Credits™
The American College of Surgeons designates this enduring activity for a maximum of 1.5 AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Of the AMA PRA Category 1 Credits™ listed above, a maximum of 1.5 credits meets the requirements for Self-Assessment.

Note: Residents will receive a Certificate of Completion.
Available Credit
- ACS Foundation
- Inclusive Excellence
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- So You Want to Be a Surgeon
- Section III
General Surgery
"General Surgery" is a discipline of surgery having a central core of knowledge embracing anatomy, physiology, metabolism, immunology, nutrition, pathology, wound healing, shock and resuscitation, intensive care, and neoplasia, which are common to all surgical specialties. A general surgeon has specialized knowledge and experience related to the diagnosis, preoperative, operative, and postoperative management, including the management of complications, in nine primary components of surgery, all of which are essential to the education of a broadly based surgeon:
- Alimentary tract
- Abdomen and its contents
- Breast, skin, and soft tissue
- Head and neck, including trauma, vascular, endocrine, congenital and oncologic disorders—particularly tumors of the skin, salivary glands, thyroid, parathyroid, and the oral cavity
- Vascular system, excluding the intracranial vessels and heart
- Endocrine system, including thyroid, parathyroid, adrenal, and endocrine pancreas
- Surgical oncology, including coordinated multimodality management of the cancer patient by screening, surveillance, surgical adjunctive therapy, rehabilitation, and follow-up
- Comprehensive management of trauma, including musculoskeletal, hand, and head injuries—the responsibility for all phases of care of the injured patient is an essential component of general surgery
- Complete care of critically ill patients with underlying surgical conditions, in the emergency room, intensive care unit, and trauma/burn units
The training program must consist of at least five years.
- Not more than 12 months may be devoted to education in a single surgical discipline other than the principal components of surgery.
- Not more than six months in total may be allocated to nonsurgical clinical disciplines such as internal medicine, pediatrics, gastroenterology, anesthesiology, or surgical pathology.
- At least 54 months (4.5 years) must be clinical surgery, with experience in endoscopy, surgical intensive care, and emergency care included under this category.
- Three of the clinical surgery years must be concerned with the principal components of general surgery.
For further information, visit the American Board of Surgery . The description of this surgical specialty was adapted from a description set forth by the American Board of Medical Specialties (ABMS).
General Surgery as a Career
General surgery is on the "cutting edge" as it continues to reinvent itself to the benefit of the surgical patient. Due to today's high-tech instrumentation and advanced technology, procedures such as major abdominal surgery are now replaced with minimally invasive laparoscopic techniques that often reduce pain, accelerate recuperation, and reduce cost without sacrificing good outcomes. Surgical research into disease processes such as immunology and genetics have redefined treatment options specific to individual patients, opening doors to better understanding the etiologies of disease and its progression. In today's environment of specialization and subspecialization, I find that as a general surgeon, my value to the patient, family physicians, and health plans grows considerably every year. General surgery affords broad, yet often very specialized training in all disciplines of surgery and medicine. After completing my residency, I became qualified to manage a wide variety of ailments, from gastrointestinal problems to endocrine surgery, from hypertensive crises to rupturing aneurysms. My training enables me to be the best person to manage patients requiring multi-system care such as major trauma, and I am frequently called upon to address complex medical and ethical issues. General surgeons often set the standard of surgical care in a community. We choose the procedures we feel most comfortable with to provide services for our patients. When patients are referred for advanced medical intervention, general surgeons are commonly the only members of the local medical staff familiar with the procedure performed or management required. And, of course, general surgeons provide life-saving procedures every day, such as appendectomy, splenectomy, or curative cancer surgery. We see the joy in our patient's face when we tell her that the breast lesion is benign, and suffer and console her when it isn't. No two days are alike. Every day is a different adventure, testing my confidence, skill, and knowledge. General surgeons are valuable not only in the eyes of the patients, but also to the health-care providers. Broad training in diverse areas keeps the general surgeon essential in today's market. General surgery continues to be a field high in public and professional demand, insuring that future general surgeons will have promising and fulfilling careers. — Gary L. Timmerman, MD, FACS, Sioux Falls, SD

IMAGES
VIDEO
COMMENTS
By Topic. Surgery General 1533; Cardiovascular Surgery ... Editor-in-Chief Eric Rubin and Deputy Editor Jane Leopold discuss research being presented at the 2024 European Society of Cardiology ...
Postoperative complications of pancreaticoduodenectomy (PD) are still a thorny problem. This study aims to verify the preventative impact of T-tube on them. Xin Luo, Xinbin Zhuo, Xianchao Lin, Ronggui Lin, Yuanyuan Yang, Congfei Wang, Haizong Fang, Heguang Huang and Fengchun Lu. BMC Surgery 2024 24:269. Research Published on: 20 September 2024.
Research Areas. As part of one the most prestigious academic medical centers in the country, the Department of Surgery at Weill Cornell Medicine undertakes a wide breadth of research each year and participates in both intramural and extramural collaborations. The research areas highlighted below are just a few of topics we are actively studying.
General Surgery - Science topic A specialty in which manual or operative procedures are used in the treatment of disease, injuries, or deformities. Questions (105)
Improving neurosurgical precision: leveraging technology for enhanced visualization and navigation of complex neuroanatomy. A multidisciplinary journal which explores surgical practices - from fundamental principles to advances in microsurgery and minimally invasive techniques. It fosters innovation and improves the cli...
Surgery is a procedure in which incision and physical manipulation are used to treat a patient with an injury or a disease. The patient's tissues are cut during this technique to permit the ...
General Surgery Research. Faculty in the division are involved in health service, education, technology, clinical trials, and translational and basic research projects. These research areas are focused on a variety topics including healthcare delivery, health policy and disease-specific gaps in knowledge. The goal of the research being ...
Selected Readings in General Surgery (SRGS ®) is a critical resource for all general surgeons. After more than 40 years, SRGS remains dedicated to ACS' mission to safeguard standards of care in an optimal and ethical practice environment. SRGS is published eight times a year and focuses on a revolving cycle of the most relevant topics in general surgery, including breast disease, colorectal ...
In the Division of General Surgery, Trauma, and Surgical Critical Care, residents have spent their research years under the mentorship Robert D. Becher, MD MS. Dr. Becher's main research focus is on the systems of care for non-trauma surgical emergencies, and how best to improve the quality and safety of general surgery operations performed non-electively, especially at the hospital-level.
The consensus was that these topics, which have been influenced by managed care and advancing technology, represent the most recent and ongoing changes in general surgery. A Medline search for the topic ambulatory surgery used the keywords "ambulatory surgery," "postoperative nausea and vomiting," "propofol," and "preemptive ...
Key Topics in Surgical Research and Methodology represents a comprehensive reference text accessible to the surgeon embarking on an academic career. Key themes emphasize and summarize the text. Four key elements are covered, i.e. Surgical Research, Research Methodology, Practical Problems and Solutions on Research as well as Recent Developments ...
Abstract. General surgery continues to evolve with advancements in techniques and strategies, presenting both opportunities and challenges for surgical practitioners. This comprehensive review ...
Updated analysis on the risks and benefits of paraesophageal hernia repair (March 2024) Paraesophageal hernia repair has not been advised for asymptomatic patients due to a high perioperative mortality relative to the risk of developing symptoms. However, in an updated Markov analysis of surgery versus expectant management for such patients ...
The future of surgical research lies, in part, in computer and visual technology. This chapter begins by describing many of the current trends in surgical research. The second half of the chapter describes the latest innovations in general surgical research. Surgeons in numerous disciplines continue to make great strides in basic science research.
The practice of surgery at Johns Hopkins is grounded in research. Our investigations drive innovations in surgical technique and patient safety, advance in the understanding and treatment of disease and trauma, and develop new technologies to help individuals and populations. We seek to further knowledge and perfect practice both in our own ...
Ten Hot Topics in General Surgery. This popular annual session provides brief presentations by experts in general surgery who discuss a specific topic in a rapid-fire format. ACS Immediate Past-President E. Christopher Ellison, MD, FACS, and Regent Kenneth W. Sharp, MD, FACS, moderated the wide-ranging session, which included presentations on:
Background. Patients requiring emergency general surgery (EGS) are known to have a high risk of death and complications [1-3] with estimates suggesting they account for 50% of all surgical mortality [].The provision of EGS service is a global public health issue, which has made it an important area of research [4, 5].In the UK, the National Emergency Laparotomy Audit (NELA) projects have ...
This allows her to shape health services research topics in national trauma and emergency general surgery systems at a national level. CAP Profile. Technology Enabled Clinical Improvement Center The Technology Enabled Clinical Improvement (T.E.C.I.) Center is a multidisciplinary team of researchers dedicated to the design and implementation of ...
The Requirements. Lancet Commission on Global Surgery estimated need of 5,000 surgeries per year per 100,000 population. 6 In India, it has been estimated that 3,646 surgeries are required per 100,000 Indian population per year. 7 Of these, 26% would be general surgical procedures, 20% would be obstetrics and gynecological surgeries, and 13% would be ophthalmological surgeries.
General Surgery Topics. Bioterrorism and Disaster Medicine. Breast Cancer. Colorectal Cancer. Inflammatory Bowel Disease. Medical Malpractice and Legal Issues. Methicillin-Resistant Staphylococcus ...
General Surgery articles covering presentation, surgical treatment, prognosis, and follow-up. Peer reviewed and up-to-date recommendations written by leading experts.
A lineup of highly regarded experts will use a lightning-round approach to explore emerging areas of interest in general surgery in the 90-minute session, "Ten Hot Topics in General Surgery." ACS Past-President E. Christopher Ellison, MD, FACS, and ACS Regent Kenneth W. Sharp, MD, FACS, will co-moderate this session, which takes place on ...
In this popular session, the panelists review 10 of the hottest topics in general surgery selected from the ACS General Surgery Communities, recent surgery meetings, and the literature. Course Outline. Approaches to Femoral Hernia Benjamin K. Poulose, MD, MPH, FACS, Nashville, TN; Pure Tissue Repair of Inguinal Hernia: Resurrection of a Lost Art
General Surgery. "General Surgery" is a discipline of surgery having a central core of knowledge embracing anatomy, physiology, metabolism, immunology, nutrition, pathology, wound healing, shock and resuscitation, intensive care, and neoplasia, which are common to all surgical specialties. The training program must consist of at least five years.